Atlanto-occipital dissociation (AOD) is a relatively rare but devastating ligamentous injury in which the skull is distracted from the cervical spine.
Many patients do not survive the initial injury due to an associated spinal cord injury. For those who survive, AOD is typically managed with posterior occipito-cervical fusion (POCF) surgery.
Yet, this surgery has potential complications and long-term consequences, including nonunion, neurovascular injury, and permanent loss of upper cervical range of motion.
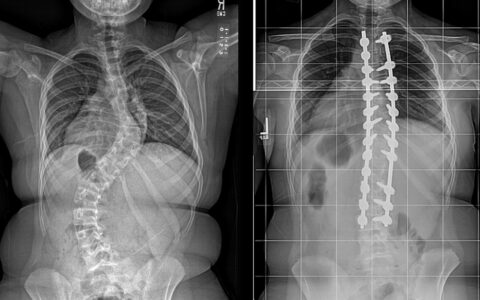
Examining alternative strategies, Jeffrey Martus, M.D., a professor of orthopaedic surgery at Monroe Carell Jr. Children’s Hospital at Vanderbilt, and his team began to question the reliance on spinal fusion surgery for pediatric AOD, considering the greater healing potential of pediatric ligament injuries. They hypothesized that halo-vest immobilization (HVI) might be considered instead in select cases of AOD.
“By virtue of anatomical predispositions, children have a greater propensity for this injury compared to adults,” Martus said.
“If we can ultimately show that outcomes are the same or improved in children when compared to upper cervical fusion, halo vest immobilization could be a viable alternative for treatment of AOD.”
Comparing Approaches
Martus and colleagues began by examining their division’s treatment strategies.
The research team performed a retrospective review over a 22-year period, reviewing records from patients under 18 years of age with unstable traumatic AOD, as defined by abnormal CT measurement criteria and MRI evidence of ligamentous injury.
Martus presented their findings at the 2023 Annual Meeting of the Pediatric Orthopaedic Society of North America.
Eleven patients made up the cohort. One died early in hospitalization after care was withdrawn due to a severe traumatic spinal cord injury. Among the survivors, six underwent HVI, and four had POCF.
An injury-associated spinal cord injury was noted in two surviving patients in each group. There were no significant differences in injury severity by CT or MRI parameters between the two groups. Length of stay was significantly shorter in the HVI group compared to the POCF group (hospital: 12.5 vs 26.3 days; ICU: 4.8 vs 17.0 days).
Martus explained the complications observed and treatment outcomes.
“Treatment-related complications occurred in three patients – two pin-site infections in HVI patients and one superficial surgical site infection in a POCF patient,” he said.
“Injury-related complications included the development of hydrocephalus requiring cerebral spinal fluid diversion with a ventriculoperitoneal shunt in one patient in each group. Unilateral cranial nerve VI (abducens) palsy was identified prior to halo application in two HVI patients – one palsy ultimately required strabismus surgery while the other resolved.”
Overall, all 10 patients survived, and the four patients with spinal cord injuries had complete neurologic recovery following treatment, Martus said. At final follow-up, the HVI patients had regained a normal level of upper cervical range of motion (average 21.6 ± 10.2° occiput-C2), without evidence of occipito-cervical instability. There were no non-unions among the POCF patients.
Importance of Early Diagnosis
According to Martus, the severity of AOD injuries can vary greatly, especially in pediatric patients. Timely recognition of this injury can be a potentially lifesaving or spinal cord-saving action.
“The dangerous instability of AOD warrants early diagnosis and immobilization, which minimizes the risk of progressive clinical deterioration,” Martus explained. “The diagnostic modality of choice is a cervical spine CT, followed by cervical spine MRI.”
Martus said that surgeons in Vanderbilt’s Division of Pediatric Orthopaedics are well-recognized experts in treating these types of traumatic injuries.
“Vanderbilt is a national leader with expertise in pediatric spine and trauma care,” Martus said.
Monroe Carell Jr. Children’s Hospital at Vanderbilt is an American College of Surgeons-verified Level I Pediatric Trauma Center and one of two pediatric trauma centers in Tennessee.
HVI: A Viable Alternative
In conclusion, Martus reported that HVI is a viable alternative to POCF but acknowledged that additional study is needed to define injury patterns most amenable to HVI.
“We recommend consideration of HVI for select cases of AOD.”
As next steps, he and his team are developing an MRI classification system to determine when POCF surgery is required.
“Stress examination with fluoroscopy under anesthesia may also be helpful to identify severe instability where fusion is necessary,” Martus added. “In the meantime, we recommend consideration of HVI for select cases of AOD.”