Medical applications of intradetrusor onabotulinumtoxin A (Botox) have skyrocketed since the early 2000s but remain fairly new in the bladder management of patients with spina bifida, particularly among pediatric patients.
Indications for choosing Botox for children over the gold standard of augmentation cystoplasty (AC) are as yet undefined, so researchers at Monroe Carell Children’s Hospital at Vanderbilt conducted a retrospective study to learn what factors led to Botox versus AC as a primary surgical treatment.
“How have we been making decisions about who gets Botox and who gets an invasive augmentation procedure?”
“We don’t have 20 years’ worth of data to know what the implications are for Botox treatment, so we’re trying to figure it out by studying recent cases,” pediatric urologist Douglass Clayton, M.D. “How have we been making decisions about who gets Botox and who gets an invasive augmentation procedure?”
Clayton was joined in the work by pediatric urologist Belinda Li, M.D., and urology fellow Leslie Peard, M.D. What they found were factors that moved the needle in each direction. Most of these were not purely medical, but more associated with the family’s preferences.
“It was really the quality-of-life measures that led families to want to pursue these larger reconstructive surgeries versus the more conservative option.”
“The key findings are that if we present patients with these different options, the main driver is the desire for independence and the desire for continence,” Peard said. “It was really the quality-of-life measures that led families to want to pursue these larger reconstructive surgeries versus the more conservative option.”
Treatment Options
Children with spina bifida struggle with a myriad of bladder conditions, including neurogenic bladder, threatening hostile bladder and incontinence. They also face a high risk of reflux into the kidney, as well as threatening urinary tract or kidney infections.
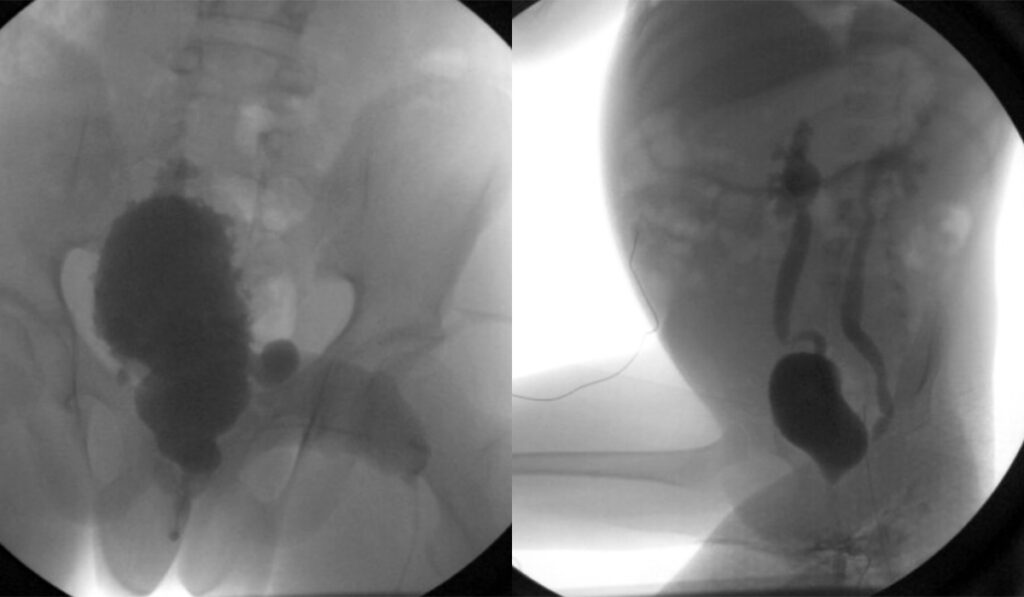
An augmentation cystoplasty is a terminal procedure in which the bladder is enlarged with a segment of small or large intestines to create an adequate reservoir for urine. A channel is also created from a segment of ileum or appendix to allow self-catheterization through the abdomen or navel, or through the urethra.
Ileovesicostomy is an option for children who may not have the capacity or willingness to self-catheterize, but those were not included in this study.
Botox’s Inroads
As with augmentation and ileovesicostomy, the primary medical indication for Botox is avoidance of renal function hazards and the potential of improving continence.
With Botox treatment, the patient is under general anesthesia for about 20 minutes while 10 to 20 injections are made into the bladder wall via cystoscopy. The goals are to relax the bladder wall and potentially add to its capacity, addressing bladder hostility. The procedure is repeated about every six months.
“Botox was FDA-approved for this use in children in 2021, but we first started using it off-label in 2012, extrapolating from what we were doing in our adult population,” Clayton said. “At first, we did maybe two or three Botox procedures a year and we probably do 100 to 120 a year now.”
Case Reviews
To find the factors that led to Botox or augmentation cystoplasty decisions, the researchers looked at the experience of Monroe Carell between 2013 and 2018, finding 14 patients who underwent primary AC and 50 who underwent primary Botox.
They identified 10 important clinical decision-making factors. Of these, the desire for independence/continence was most highly associated with augmentation surgery, with reduced capacity also reaching significance. Significantly associated with choosing Botox were, in order, end-filling pressure (EFP) ≥40 cm H2O; rising slope; physician-perceived bladder hostility; trabeculation; and reduced capacity.
Heart of the Conversation
Clayton says the augmentation procedure requires confidence that the patient will reliably catheterize. If they don’t, they risk dangerous complications, even years after their procedure. Botox is its own commitment, but there is always the option to switch and have surgery.
“We don’t see a lot of medical reasons that qualify them for one or the other, so it is a patient preference thing,” Clayton said. “But if they are considering surgery, we will have multiple conversations with the patients and their families before moving forward.”
Mining Urodynamics
With no risk-scoring system in the pediatric literature, the team at Monroe Carell has developed its own, categorizing patients into groups with low-risk, intermediate-risk, or high-risk urodynamics.
Clayton is also working on a urologic management protocol through the nine-center UMPIRE study, reviewing every urodynamic study and following children prospectively to determine how best to care for their bladder and protect their kidneys.
“Interpretation of urodynamics, which are like an EKG for the bladder, has been highly variable,” he said. “This is a place where AI may be really useful in establishing more uniform medical indications for each procedure, which will in turn feed into the conversations we have with families.”
He is also looking at a study to see how the rise in Botox use has affected the need for augmentation cystoplasty.
“The natural conclusion is that if you’re doing more Botox and you’re doing it earlier, you’re treating bladder dysfunction earlier,” he said. “This may avoid the need for augmentation cystoplasty, because you’ve effectively managed the bladder better with Botox.”
He anticipates an eventual formulation of Botox that is deliverable without injection.
“Those aren’t anywhere close to prime time, but until then, I do think we’ll do a lot more injections of Botox in adults and children without general anesthesia,” he said.