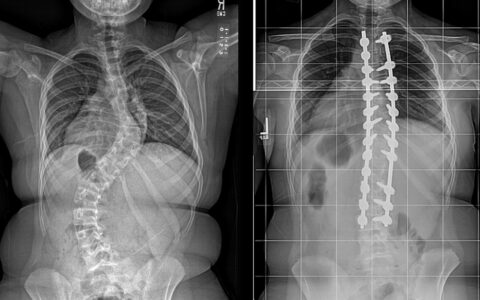
A new study from the Vanderbilt Center for Bone Biology examines the metabolic processes by which osteoblasts grow and proliferate in young and old mice, demonstrating differences that may account for loss of bone mass in older people.
“Very little has been studied on the aging of bone cells relative to their metabolic function,” said molecular biologist Elizabeth Rendina-Ruedy, Ph.D., principal investigator on the study. “Other research has shown that older osteocytes accumulate lipid droplets, but we wanted to see how this relates to the aging process.”
“Other research has shown that older osteocytes accumulate lipid droplets, but we wanted to see how this relates to the aging process.”
By comparing the osteoblasts of young and old mice in vitro, researchers observed that young osteoblasts are more omnivorous, using multiple nutrients for their survival, while osteoblasts in geriatric mice more heavily consume fatty acids. The limited diet of older mice promotes mitochondrial dysfunction and apoptosis, and reduced bone density. The team published their work in Aging and Disease.
“In our murine model and in human cells, we found vastly different metabolic profiles between young versus aged osteoblasts at both the transcript and activity level,” Rendina-Ruedy said.
Further, in the bone cortex of mice, Rendina-Ruedy’s team confirmed that the quantities of lipid species (i.e., triglycerides, cholesteryl esters and fatty acids) in the osteoblasts varied significantly within similar-aged mice, raising the question of why, for some, individual bone health deteriorates more rapidly than in others.
Double-Edged Sword
Rendina-Ruedy and her team performed seahorse flux assays, where single nutrients and combinations of nutrients were introduced or withheld. In young mice, they found osteoblasts to be preference-neutral, readily and interchangeably taking up glutamine, glucose, or oleic acid in their metabolic processes. In the aged mice, however, the osteoblasts were less flexible, having an affinity for fatty acids and therefore accumulating lipids and triglycerides.
“We suspect fatty acids are very helpful to a certain point, if there are too many, they may overwhelm the mitochondria, making them more prone to proton leakage and reactive oxygen species formation.”
“In young mice, lipid accumulation progresses slowly during osteoblast differentiation,” Rendina-Ruedy said. “But in older mice, aging results in the accumulation of lipid content in both bone cortex and bone marrow stromal cells.”
Paradoxically, lipid droplets can protect osteoblasts from the higher oxidative stress that comes with aging, but In order to utilize the stored lipids for fuel, the cells have to make a metabolic energy shift from glycolysis to oxidative phosphorylation. This triggers formation of reactive oxygen species, which are damaging or fatal to the cell.
“We don’t really know why the osteoblasts from older mice are pulling in a bunch of fatty acids, or what is regulating this switch,” Rendina-Ruedy said. “While we suspect fatty acids are very helpful to a certain point, if there are too many, they may overwhelm the mitochondria, making them more prone to proton leakage and reactive oxygen species formation. This may render them dysfunctional, leading to greater osteoblast death.”
Genetic Clues
By studying the transcriptome, the researchers identified three of the most highly-regulated metabolic genes in bones from aged mice – two genes involved in lipid uptake, Apol11a and Apol10a, and one with lipid metabolism, Fgfbp3.
Aged bones also demonstrated increased expression of genes involved in fatty acid uptake, fatty acid storage/lipid droplet biosynthesis, and fatty acid oxidation. These lipid-related changes were also associated with increased oxidative stress. Thus, while esterification of fatty acids to lipids can be protective, during aging it appears to contribute to also increase stress, thereby reducing bone formation by the osteoblast.
Toward Treatments
Bisphosphonates, the first-line treatment for osteoporosis, works by suppressing bone resorption by promoting osteoclast apoptosis. Rendina-Ruedy is looking into how bisphosphonates might also directly impact osteoblasts, as their mechanism of action involves lipid metabolism.
Supplemental or alternative therapies are still needed, as some associations between bisphosphonates with jaw osteonecrosis and with brittleness have been found with long-term use.
To work toward new treatments, Rendina-Ruedy and her team are researching the appropriate role and healthiest quantity of lipids and fatty acids in osteoblast metabolism. In a new, complementary study, she describes the lipid droplet itself, what it does in the osteoblast, and how it provides fatty acids for ATP production that is needed to form bone.
This study, coupled with the current one, suggests that reduced bone formation associated with aging could be a function of altered metabolism and reduced bioenergetic capacity, or cellular energy production. In short, you can form bone, if and only if, the osteoblast has the necessary energy, she says.
“We know that too much of it is bad and too little of it is bad, but what is the ideal amount? It’s sort of been a black box,” Rendina-Ruedy said. “Once we have connected more of the dots, it may help us answer the questions of what we can eat to slow osteoporotic changes and whether we can couple that with therapeutic regimens to prevent or stave them off.”