ROSA Brain, a robotic assistance platform for surgery, offers neurosurgeons a minimally invasive approach to precision brain mapping and the correct placement of their instruments.
“It acts as a system for us to make surgical plans accurate, precise and safe, and we also use it for treatment,” said Robert Naftel, M.D., a pediatric neurosurgeon at Monroe Carell Jr. Children’s Hospital at Vanderbilt.
Naftel, the first neurosurgeon to perform a ROSA Brain-guided procedure in Tennessee, says that of the system’s many benefits, the greatest is its power to “leverage the abilities of our most valuable resource – our talented, deeply caring neurosciences team.”
“ROSA allows us to turn this clinical acumen into action by performing safe, precise, individualized surgical care for our patients.”
How It Works
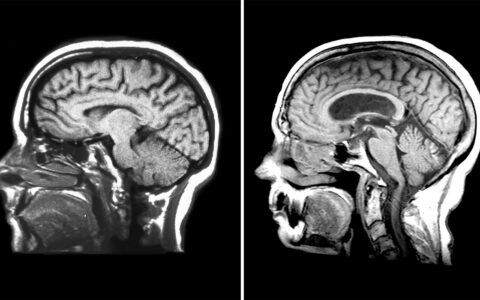
ROSA Brain, developed by Zimmer Biomet Robotics in France, supports stereotactic operations by eliminating the need for frames or external, fixed landmarks. Instead, a robotic arm moves along six axes, guided by preoperative reference images.
The manufacturer calls it “a kind of ‘GPS’ for the skull” that can assist surgical planning and “keyhole” interventions.
The robotic arm’s dexterity helps neurosurgeons implant electrodes and perform other procedures with unprecedented precision. It also provides real-time haptic feedback to keep surgeons away from surrounding tissues.
Guiding Seizure Diagnostics
Epilepsy cases are the most common procedures he and his colleagues perform, Naftel said.
“ROSA plays an integral part in our neurosurgical care for patients with epilepsy. We use it innumerable times each year,” he said.
Neurosurgeons can use ROSA Brain to inform stereoelectroencephalography (SEEG) and place electrodes into areas of the brain where seizures appear to originate.
“The most common application for ROSA Brain has been in treating medically refractory epilepsy,” Naftel said. “When children are no longer responding to epilepsy medications, we consider surgical options by determining where in the brain the seizures originate.”
Tapping into Diverse Sources of Information
Scalp EEGs and MRIs can sometimes locate seizure sources, but typically more invasive diagnostics are needed.
“ROSA allows us to turn this clinical acumen into action by performing safe, precise, individualized surgical care for our patients.”
Naftel’s team may use data from combinations of video EEG, MRI, PET, SPECT, MEG, physical exams and neuropsychological testing to form hypotheses about where the seizures are coming from. They then import a patient’s MRI into the ROSA Brain software and together, with information from these other sources, develop a personalized plan for electrode placement.
“All this planning work occurs ahead of the surgery such that on the day of the surgery, plans are already loaded into the robot and it’s just a matter of registering the robot to the child’s anatomy and inserting the electrodes to discover epilepsy onset zones in the brain,” Naftel said.
Greater Precision, Shorter Procedure
ROSA Brain can guide surgeons through electrode entry, trajectory and termination. “It provides submillimeter accuracy and stability we would not have with the frames or other devices we used to use,” Naftel said.
Once the seizure locations are confirmed by an electrode, neurosurgeons may remove or ablate the tissues where they originate.
With ROSA Brain, Naftel’s surgeries have shortened from four to five hours down to about three, so children are under anesthesia for a shorter time. Improved precision during electrode placement also helps avoid contact with critical brain structures and blood vessels.
Expanding Applications
Versatility is part of ROSA Brain’s appeal; the system can assist with biopsy and treatment of both brain tumors and blood vessel abnormalities, such as cavernous malformations.
“It’s different than other robotic surgical systems, like the da Vinci® systems, where a robot has instruments to perform procedures. With ROSA Brain, it’s all about lining up trajectories and acting as a platform for us to perform procedures,” Naftel said.
Neurosurgeons are also using ROSA Brain in guided biopsy, shunt placement and deep brain stimulation. “The robot can also be used to guide laser treatments, and all this is done minimally invasively,” Naftel said. “We’re never drilling a hole in the skull more than a few millimeters wide.”