The body efficiently regulates biomineralization so that it occurs in bones and teeth, where it imparts strength and structure, but not in soft tissues, where it can impede function, resulting in patient pain and disability.
“These biomineralization regulatory mechanisms are vital after an injury occurs,” said Jonathan Schoenecker, M.D., the Jeffrey Mast Associate Professor of Orthopaedics at Vanderbilt University Medical Center. “In an ‘isolated’ injury like a broken arm or leg, the mechanisms promote rebuilding of the damaged bone while simultaneously inhibiting it in the damaged muscle.”
Polytrauma Disrupts the Process
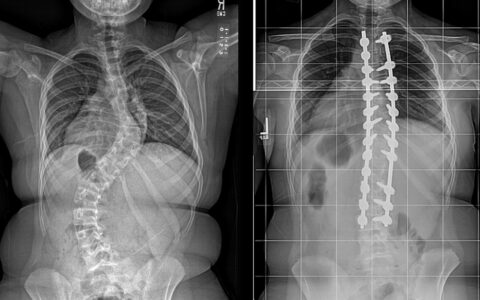
Paradoxically, though, after a polytraumatic injury, one that includes damage to both bone and muscle in a limb and another severe injury such as a burn, these mechanisms often become dysregulated, Schoenecker explained.
This can lead to reduced biomineralization in bone and increased biomineralization in soft tissues, pathologic events that can in turn foment problems including bone loss, impaired fracture healing and soft tissue calcification.
“To improve outcomes for patients who’ve experienced a polytraumatic injury, we need therapeutics that can help regulate biomineralization to the bone and block it within soft tissues,” said Stephanie Moore-Lotridge, an assistant professor of orthopaedic surgery and who collaborates closely with Schoenecker.
A Unified Theory of Calcification Disease
Clinical observations led the research team to hypothesize that the pathologies of dysregulated biomineralization may be mechanistically linked, Schoenecker stated. While essential regulators of biomineralization have been defined in specific anatomic systems, such as bone or muscle, the team is pioneering the study of how these mechanisms function across tissue types (bone, muscle, skin and tendons).
By better defining causes of dysregulated biomineralization after polytraumatic injury, the group foresees developing treatments to restore healthy biomineralization.
Mimicking the Clinical Condition
“Our laboratory focuses on developing and validating murine models that mimic the conditions I treat as an orthopaedic surgeon,” Dr. Schoenecker said. For example, the team has developed a clinically relevant mouse model of polytrauma and novel techniques to sensitively measure ongoing changes in biomineralization.
The group’s recent article in Bone Reports is one of the first publications to show temporal linkages between osteoporosis and muscle calcification after polytrauma. “We were able to show a temporal connection in these changes of biomineralization by using sensitive, longitudinal monitoring in our polytrauma model,” Moore-Lotridge said.
The team found that significant loss of bone was detectable as early as 3 days post-injury and progressed through 28 days post-injury. During the same period the researchers observed muscle calcification starting 7 days post-injury.
“Together, these observations further support our laboratory’s hypothesis that there is a shared, mechanistic link between pathologic loss of biomineralization from the bones and the accumulation of minerals in soft tissues after a polytrauma,” said Schoenecker.
Pharmaceutical Rebalancing Poses Challenges
“When we’re looking to pharmacologically correct dysregulated biomineralization following a polytrauma, an ideal treatment would prevent the biomineralization in soft tissues, yet still be good for bone health and repair,” Schoenecker said. While drugs such as anti-bone morphogenic protein (BMP) may effectively prevent ossification in muscle compartments after a polytraumatic injury, they can also impede fracture repair.
This pharmacologic challenge illustrates why the group’s new animal model of polytrauma with dysregulated biomineralization are essential, Moore-Lotridge explained. “This model lets us assess new treatments aimed at preventing pathologic biomineralization, and also lets us assess how these treatments may affect ongoing tissue repair,” she said.
Ongoing Investigations and Future Trials
In prior work, the Schoenecker team had demonstrated that the enzyme plasmin helps prevent calcification in soft tissues; is essential for fracture healing; and helps protect against diseases such as osteoporosis.
“Given that we know that plasmin activity is impaired in severe injury, these findings suggest that therapies that boost plasmin activity may prevent soft tissue calcification without hindering bone repair after a polytraumatic injury,” Schoenecker said. The team is now testing this hypothesis with funding from the National Institutes of Health and Department of Defense.
Repurposing Drugs Already Approved
The group is investigating the repurposing of drugs that already have FDA approval, including bisphosphonates, for their potential to treat dysregulated biomineralization. Bisphosphonates possess anti-mineralization capacity akin to that of their parent molecule, pyrophosphate.
Schoenecker’s group has previously published reports demonstrating pyrophosphate’s role in protecting muscle from aberrant mineralization after injury. They are continuing to investigate if bisphosphonates can be used following a polytrauma to treat dysregulated biomineralization.
Timing Proves Crucial
“Time relative to the injury is essential for deciding when to administer therapeutics, such as bisphosphonates,” Moore-Lotridge said, describing a key finding of the recent study in Bone Reports. “We’re working to identify the pharmacologic window after polytraumatic injury during which treatments can help limit muscle calcification, without hindering bone healing.”
Muscle, bone, skin, tendons, etc., all heal simultaneously after polytrauma, she explained, so the researchers must weigh the effects of treatments on multiple tissues. “The goal is to optimize treatment for all healing tissues, not to sacrifice one at the expense of improving another,” Schoenecker said.