No specific guidelines currently exist for the diagnosis and management of fetal closing gastroschisis. In a study published in the Journal of Perinatology, a team of researchers took significant steps to fill this gap, comparing outcomes of different treatment approaches and the prognostic capability of prenatal imaging.
Closing gastroschisis is a rare (6 percent) complication of gastroschisis, a complex fetal disorder where intestines herniate through a defect in the abdominal wall. When this occurs, timely clinical intervention is needed to prevent serious sequelae, including mortality.
“The ongoing challenge is to weigh the risks of prematurity with the risks of continuing a pregnancy with closing gastroschisis. The latter include bowel injury leading to short gut syndrome, oligohydramnios or low fluid, higher risk of abnormal fetal testing and fetal distress, and a higher risk of stillbirth,” said Harold Lovvorn, M.D., a pediatric surgeon and professor of pediatrics at Vanderbilt University Medical Center, who participated in the study.
“If we can predict which fetuses are at risk for this catastrophic event, then we can better identify patients for earlier delivery with the goal of preventing loss of bowel length.”
Study team member Lisa Zuckerwise, M.D., an assistant professor in the Division of Maternal Fetal Medicine at Vanderbilt, performed retrospective ultrasound analyses that may be predictive of closing gastroschisis. “We have not yet figured out how to prenatally determine which patients are at risk for poorer outcomes like closing gastroschisis,” Zuckerwise said. “We are seeking evidence of a ‘safety zone’ to help guide our teams prenatally.”
Strategies to Avoid Poor Outcomes in Gastroschisis Cases
Gastroschisis cases (approximately 1 in 2,000 pregnancies) are classified as uncomplicated, complicated, or closing. Most are relatively innocuous, Lovvorn says, and babies undergo vaginal delivery followed by postnatal surgical repair.
In complicated gastroschisis, there is associated bowel atresia, but this is often limited in size and extent. “Gastroschisis in itself has a great prognosis. In the vast majority of patients, we can reassure parents that the outcome will be favorable with minimal long-term consequences,” Zuckerwise said.
In closing gastroschisis, however, the abdominal fascia can strangulate the protruding bowel, leading to a significant loss of blood supply to the organ, and potential necrosis. Rarely, the stricture amputates the bowel, which floats in the amniotic sac. “If we can predict which fetuses are at risk for this catastrophic event, then we can better identify patients for earlier delivery with the goal of preventing loss of bowel length,” Zuckerwise explained.
Outcomes Inform Planning
The researchers’ two-part study evaluated neonatal management and prenatal predictors. “A key study goal was to identify the highest-risk group so we can prepare the best surgical strategy in advance of their delivery,” Lovvorn said.
“My goal was to see if we could identify, by gestational age, parameters for defect size that may be predictive for closing gastroschisis.”
The study team looked at 197 cases of gastroschisis, 18 of which were closing gastroschisis, first comparing the current standard approach of resecting the compromised bowel to a novel method of intracorporeal “parking.” In parking, Zuckerwise explained, the bowel is preserved by suturing it to the neonate’s abdominal wall for potential use in later intestinal remodeling. The researchers found no significant outcome differences for the approaches.
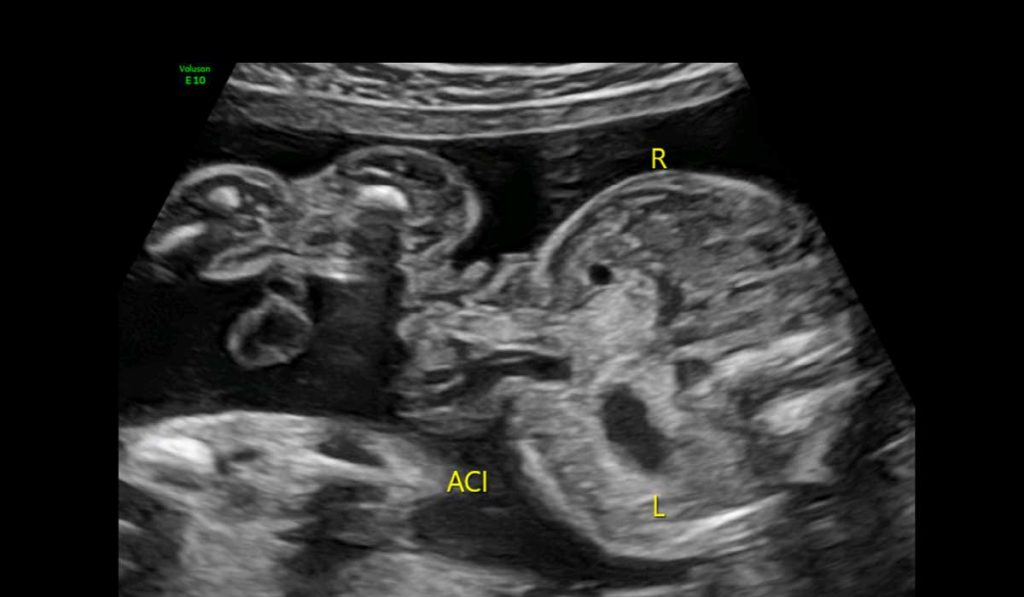
To investigate prenatal predictors of closing gastroschisis, Zuckerwise examined serial ultrasound exams from 33 patient records – 11 with an ultimate diagnosis of closing gastroschisis, and 22 with uncomplicated or complicated gastroschisis. “My goal was to see if we could identify, by gestational age, parameters for defect size that may be predictive for closing gastroschisis,” Zuckerwise said.
Zuckerwise found that fetuses with closing gastroschisis began showing progressive defect narrowing to ≤8 millimeters after 30 weeks gestation. Patients with larger holes at this point in pregnancy had a 98 percent chance of delivery without progression to closing gastroschisis. “This cutoff enables us to both prepare as a medical team and prepare the parents for what may lie ahead,” she said.
Replication Sought
Lovvorn and Zuckerwise eagerly anticipate the Fetal Center at Vanderbilt’s planned participation in a randomized trial of different delivery timing approaches for these patients.
In the meantime, they are routinely assessing abdominal defect size prospectively through ultrasound. “If we measure from the transverse view at the level of the defect in every case, and repeat that progressively with standard caliper placement, we can accrue data that either supports or questions our initial findings,” Zuckerwise said.