“Tibial plateau fractures are one of the few injuries that encompass all aspects of orthopaedic trauma,” said William T. Obremskey, M.D., orthopaedic trauma surgeon at Vanderbilt University Medical Center. “They deal with injury including skin and soft tissue, bone, cartilage, ligaments and tendons.”
Obremskey is researching treatment challenges associated with tibial plateau fractures and strategies to manage complications. He explored this topic at the most recent meeting of the Orthopaedic Trauma Association, joined by a panel of experts.¹
Tailoring Treatments
“Fracture patterns may require posterior approaches, medial, lateral or a combination.”
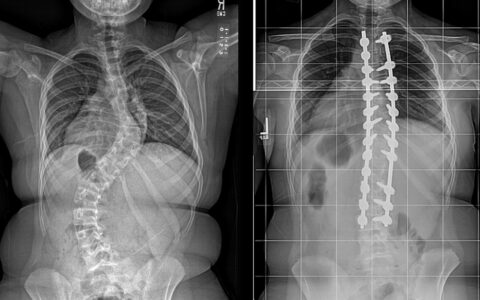
Complex tibial plateau fractures typically result from high-energy impact, either alone or combined with other stress on the knee joint. Variable force geometry makes each fracture slightly different. Fractures may be lateral, medial, biocondylar, and may not fit traditional Schatzker classifications.
Treatments involve both acute and delayed intervention. In some cases, tibial plateau fractures will heal non-operatively or only require arthroscopic fixation. Other patients may undergo staged surgical joint reduction combined with lengthy physical rehabilitation to restore the lower limb axis and range of motion.
There may be challenges deciding which treatment is most appropriate for which fracture. Said Obremskey, “Fracture patterns may require posterior approaches, medial, lateral or a combination to reduce and stabilize fracture components.”
Managing Infection
Challenges with tibial plateau fracture persist long after treatment. “Treatments are associated with significant complication rates,” Obremskey said. “Infection rates can be as high as 20% in biocondylar tibial plateau fractures.”
In a recent review article of fracture-related infections, Obremskey and colleagues found 64% involved the tibia. Some tibial plateau fractures also cause compartment syndrome that can further raise the risk of infection and impede healing.
In addition to perioperative or local antibiotics to drive down infection rates, Obremskey advises: “Avoid use of an external fixator if you can with staged fixation or early fixation. External fixators are necessary at times due to severe swelling or fracture complexity. External fixator pins should be removed prior to fixation as pin sites are colonized and can increase risk of MRSA infection.”

Standardizing Guidelines
With so many variables, navigating treatment guidelines for tibial plateau fractures is difficult—particularly as related to handling complications.
“There is a lack of standardized guidelines with respect to diagnosis and treatment of fracture-related infection,” Obremskey said. “The best approach is ‘stack the deck’ in your and the patient’s favor by utilizing all opportunities to decrease infection risk.”
Obremskey has been working to identify factors that can help predict which patients are at highest risk of complications from tibial fractures. His studies could help care teams tailor surgery and rehabilitation protocols to address challenges inherent to a patient’s fracture. “The more we discuss these challenges, the better we can serve our patients,” he said.