“Prior studies have quantified the harms of prostate cancer treatment. But they have been difficult to execute. We wanted to include newer treatments in the comparison and study a more diverse population.”
Understanding the comparative adverse effects of approaches to localized prostate cancer treatment can support informed decision making and, as a result, may lead to better patient outcomes. With this in mind, researchers at Vanderbilt University Medical Center designed an ambitious, prospective, cohort study — the Comparative Effectiveness Analysis of Surgery and Radiation, or CEASAR, study — to compare functional outcomes and adverse effects associated with radical prostatectomy, external beam radiation therapy (EBRT) and active surveillance.
“Prior studies have quantified the harms of prostate cancer treatment,” said Daniel Barocas, M.D., associate professor of Urologic Surgery at Vanderbilt and co-principal investigator of the study. “But they have been difficult to execute. We wanted to include newer treatments in the comparison and study a more diverse population.”
David Penson, M.D., Chair of Urology and director of the Vanderbilt Center for Surgical Quality Outcomes Research, was co-principal investigator of the study and senior author of the results published in JAMA. The study was a collaboration with investigators from the University of Texas, the University of California San Francisco, Emory University, the University of California Irvine, the University of Southern California, the University of Utah, Rutgers University, Louisiana State University and Tennessee Valley Veterans Administration Health System.
Cohort
The study involved 2,550 men (≤80 years) diagnosed in 2011-2012 with clinical stage cT1-2, localized prostate cancer, with prostate-specific antigen levels less than 50 ng/mL and enrolled within six months of diagnosis. The mean age was 63.8 years; 74 percent of participants were white. 55 percent had intermediate- or high-risk disease, of whom 1,523 (59.7 percent) received radical prostatectomy, 598 (23.5 percent) EBRT, and 429 (16.8 percent) active surveillance. Men in the EBRT group were older (mean age, 68.1 years versus 61.5 years) and had worse baseline sexual function than men in the radical prostatectomy group.
Measures
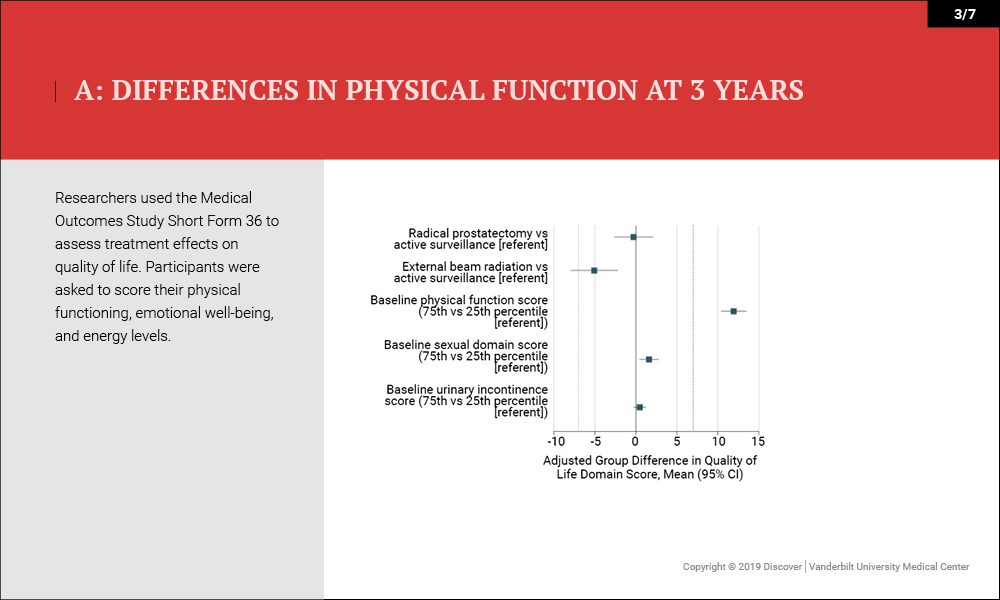
Outcomes were measured by patient-reported function on the 26-item Expanded Prostate Cancer Index Composite (EPIC) 36 months after enrollment. Higher domain scores (range, 0-100) indicated better function. “Minimum clinically important difference” was defined as 10 to 12 points for sexual function, 6 points for urinary incontinence, 5 points for urinary irritative symptoms, 5 points for bowel function and 4 points for hormonal function.
Results
In the cohort of men with localized prostate cancer, the following outcomes were reported:
- Sexual Function – Radical prostatectomy was associated with significant declines in sexual function compared with external beam radiation therapy (−11.9 points on the 100-point scale) and active surveillance (−16.2 points) at three years. Active surveillance was not clinically significant (−4.3 points).
- Urinary Incontinence – Radical prostatectomy was associated with worse urinary incontinence than EBRT (−18.0 points) and active surveillance (−12.7 points) but was associated with better urinary irritative symptoms than active surveillance (5.2 points).
- Bowel/Hormone Function – No clinically significant differences for bowel or hormone function were noted beyond 12 months.
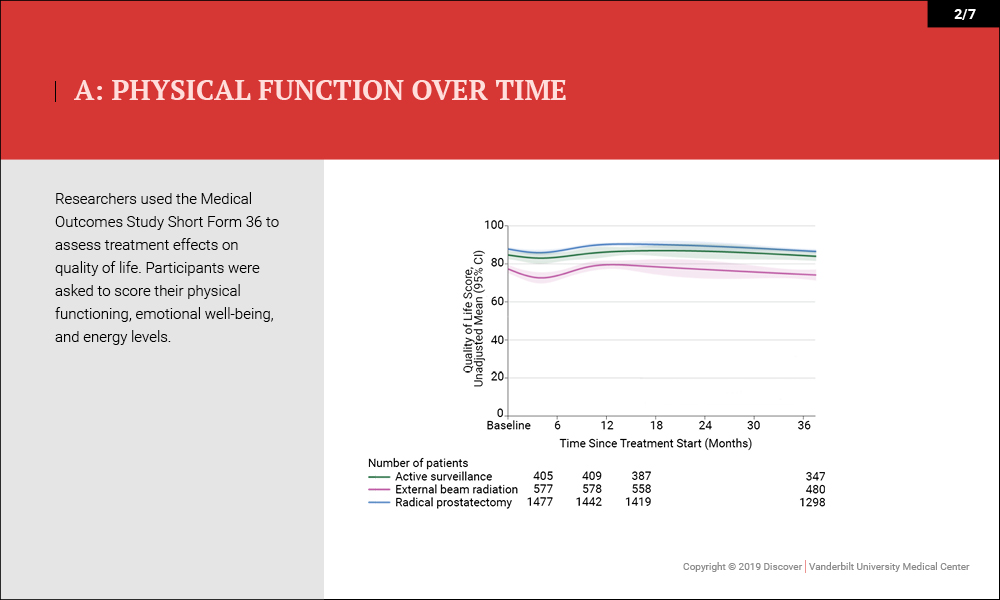
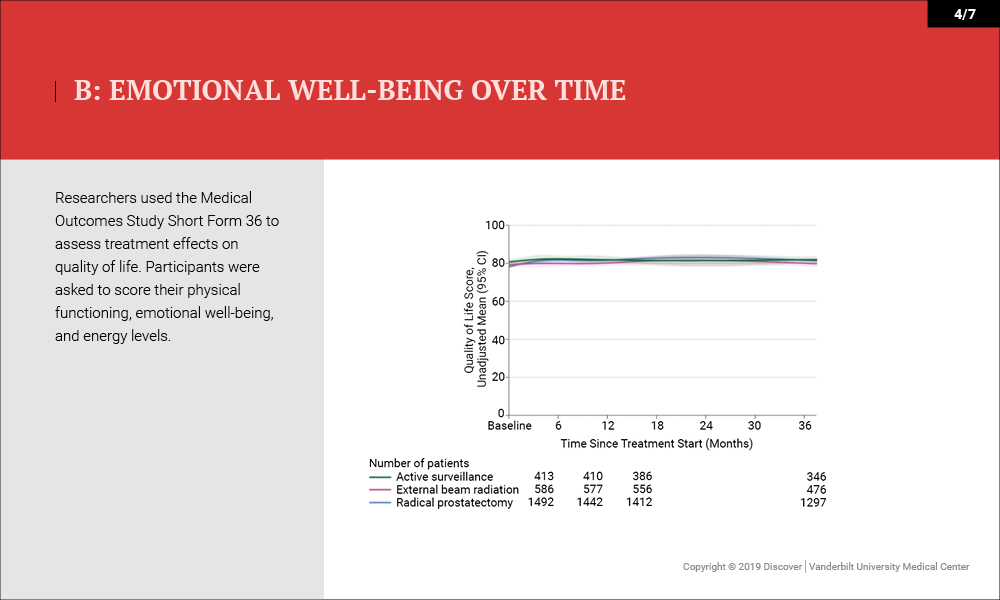
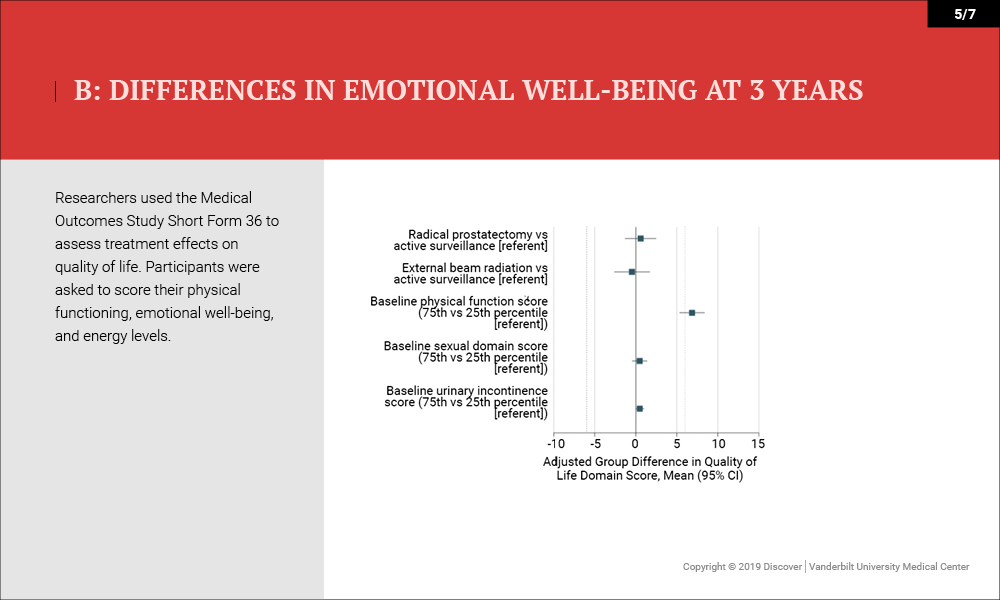
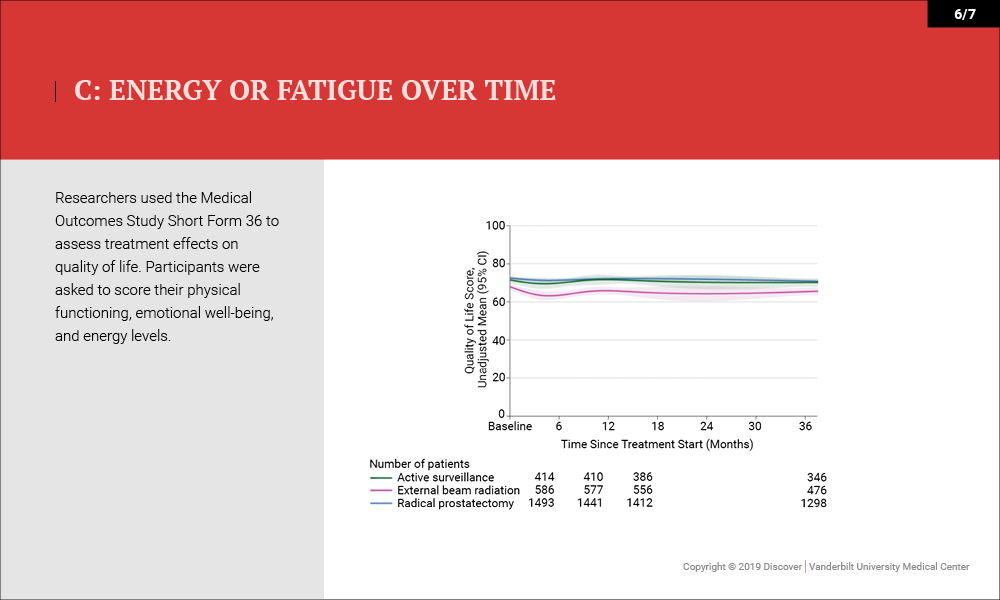
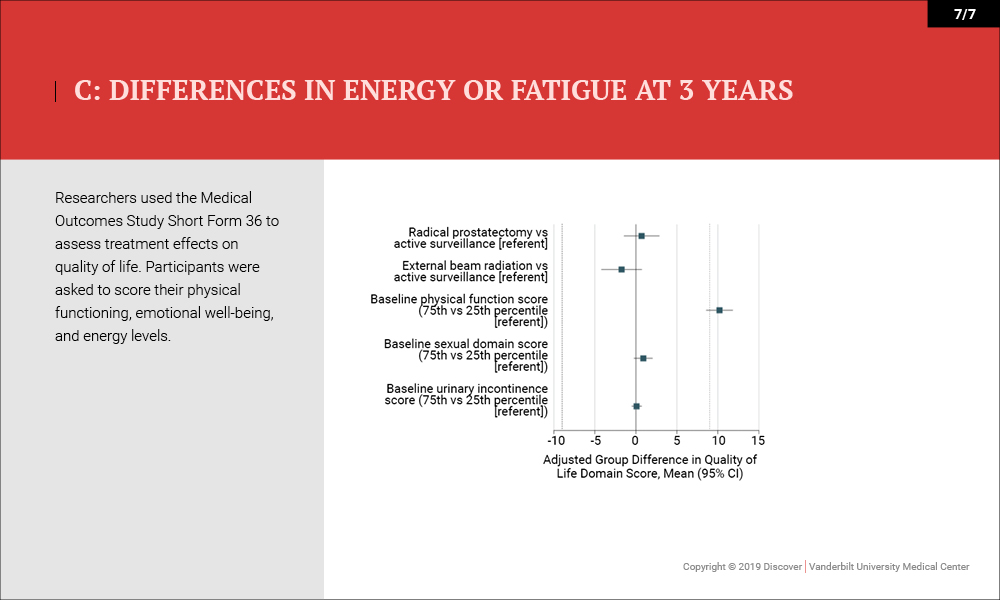
- Quality of Life/Survival – No differences in health-related quality of life (physical functioning and energy or fatigue) or disease-specific survival (three deaths) were noted (99.7-100 percent).
Conclusions
The study demonstrated the frequency and severity of the adverse effects of contemporary treatments for prostate cancer and the likelihood of preserved global quality of life regardless of treatment, thus providing a basis for shared decision making. It may inform future research on personalized risk assessment, tools to facilitate shared decision making and other patient-centered outcomes.
“We hope these findings will facilitate counseling regarding the comparative harms of contemporary treatments for prostate cancer,” said Barocas.
“The findings of this study underscore the importance of shared decision making in the setting of localized prostate cancer,” said David Penson. “They really highlight the need to reserve aggressive therapies, like surgery or radiation, for patients who need them most. In patients with less-aggressive, low-grade disease, active surveillance is probably a better way to go.”