The CDC has released its first clinical recommendations for treating children with mild traumatic brain injury (mTBI), representing a comprehensive evaluation of 25 years of research. The guidelines were published in JAMA Pediatrics. They include 19 sets of clinical recommendations covering diagnosis, prognosis and management and treatment.
“A lot of effort went into this,” said Andrew Gregory, M.D., a sports medicine specialist and co-director of the Vanderbilt Sports Concussion Center. “It’s a comprehensive document, but it includes many practical, helpful tools.” Gregory served on the CDC working group that developed the mTBI guidelines.
Discoveries: Dr. Gregory, before we talk about specific recommendations in the guidelines, how were you involved in their development?
Gregory: I was asked to represent the Academy of Pediatrics as a part of the work group developing these guidelines for the CDC. It was an extensive review. I served on the group reviewing all diagnostic studies on pediatric concussion, culling through all those articles to find the best information.
Discoveries: What motivated the CDC to finally offer guidelines for pediatric mTBI?
Gregory: There had been recommendations published before, but not from an authority like the CDC. There was a strong need for detailed guidelines that are specific for pediatrics.
Discoveries: What research in particular had enough significance to make its way into the guidelines?
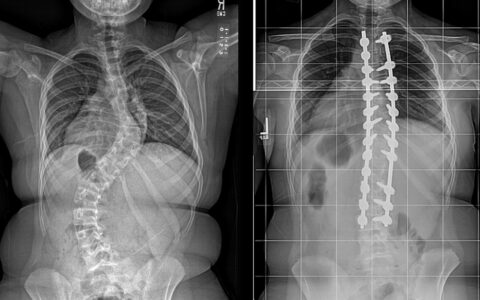
Gregory: For other forms of traumatic brain injury, imaging is of key importance because you can see fractures and you can see bleeds. The challenge with mild traumatic brain injury, or concussion, is that those objective measures seen in standard imaging are not available. Certainly, we looked at some of the newer types of imaging like functional MRI or diffusion tensor imaging, but we also looked at a lot of more standard outcome measures like concussion symptom checklists, neuropsych testing and EEG.
Discoveries: Was the choice of term “concussion” versus “mild traumatic brain injury” part of the discussion?
Gregory: The definition of concussion can be challenging. We used concussion in this setting as synonymous with mild traumatic brain injury, which is essentially image negative traumatic brain injury. There’s no fracture and no bleed. Our search terms included related phrases like closed head injury and traumatic brain injury, more generally.
Discoveries: There are 19 sets of recommendations in the guidelines. What will be the most useful elements for physicians who are diagnosing and treating mTBI?
Gregory: The work group made a strong effort to distill down the recommendations, even creating a one-page handout for clinicians. They’ve even identified standardized tools like the sideline assessment of concussion, or SCAT5. One of the best things the CDC is making available is their own training program for clinicians. That’s available on their website for free.
“It’s important to be aware that while concussions happen in sports settings, they can happen anywhere.”
Discoveries: Obviously, the CDC is taking many steps to ensure these guidelines reach clinicians. What are your further thoughts on getting these recommendations into clinical practice?
Gregory: It’s a great question. When we think about who needs this information, we include more than just primary care providers, athletic trainers, physical therapists and other physicians who work with athletes. Sports are one setting where concussions happen, but this is also important for providers in urgent care, ERs, primary care offices, etc. We need to reach all of these providers and let them know that this is the best science. I’m not sure there is one best approach, but the guidelines will need to be presented at educational meetings and other events for different provider groups.
Discoveries: How will these guidelines relate to the types of complex cases you’re seeing at the Sports Concussion Center?
Gregory: We already incorporate the best practices recommended by the guidelines. We require yearly education — we all take the provider course issued by the CDC every year. We’re lucky in that we have a great team that includes physicians, neuropsychologists and athletic trainers who are experts in this area. As I noted earlier, one of our most important roles will be dissemination of this information.
Discoveries: What’s happening now in concussion research or innovation that will be influential going forward?
Gregory: One of the nice things about our dedicated concussion program is that we are approached by industry for testing new products. For example, we’ve assessed several balance testing innovations that didn’t turn out significant results. The most recent innovation uses audio signal between your ears. It was invented for detecting increase in intracranial pressure, but it may have potential to detect concussion changes.
It is definitely a goal to develop a fairly simple device that could be used to test for concussion on the sideline, or even in an urgent care setting. The jury is still out, but it’s nice to be involved in those efforts to advance the field.
Discoveries: As a physician who consults for a number of sports teams, how do you see your peers in athletics using these guidelines?
Gregory: If you are familiar with concussion, this may not change a lot about your current practice. It does give you the science to back up what you’re doing. It also provides a framework to ensure everybody is following the standard and practicing the same way. Dissemination of the information is paramount, including requiring that medical practitioners be trained in current management standards.
Discoveries: Currently, laws about training are at the state level?
Gregory: There are laws in all states, but there is no federal law. And the state laws are all different. I think all physicians and providers should be required to have training if they’re managing kids with concussion.
Discoveries: Sports like football receive the most attention. Where else are child concussions happening frequently?
Gregory: As kids get older, it is more likely the injury is related to a sporting activity. Younger children are more likely to be injured in a recreational activity, whether that would be bikes, scooters, trampolines or monkey bars. It’s important to be aware that while concussions happen in sports settings, they can happen anywhere.
Discoveries: That suggests the importance of disseminating the guidelines beyond just providers involved in formal athletics.
Gregory: That’s right. Parents, athletes, coaches, teachers and school administrators all need to be aware. The CDC has recognized the scope of that, which is why they’re offering free online training for all of those groups.
Discoveries: Lastly, how do these guidelines for children differ from those for adults?
Gregory: The Concussion in Sport Group has published guidelines for adults with a scientific basis. The section for children has been limited, which is why the CDC effort will help fill an important void. As to how the science and guidelines differ, it does appear that kids are more likely to get concussion than adults. It also appears they take a little bit longer to recover. For example, one of the challenges is neuropsych testing: kids are improving their baseline year to year, whereas in adults our baseline is flat. There are certainly unique challenges in managing concussions in kids.
Discoveries: Thanks for talking with us today, and thanks for your role in developing the new CDC guidelines.
Gregory: Thanks for the opportunity.