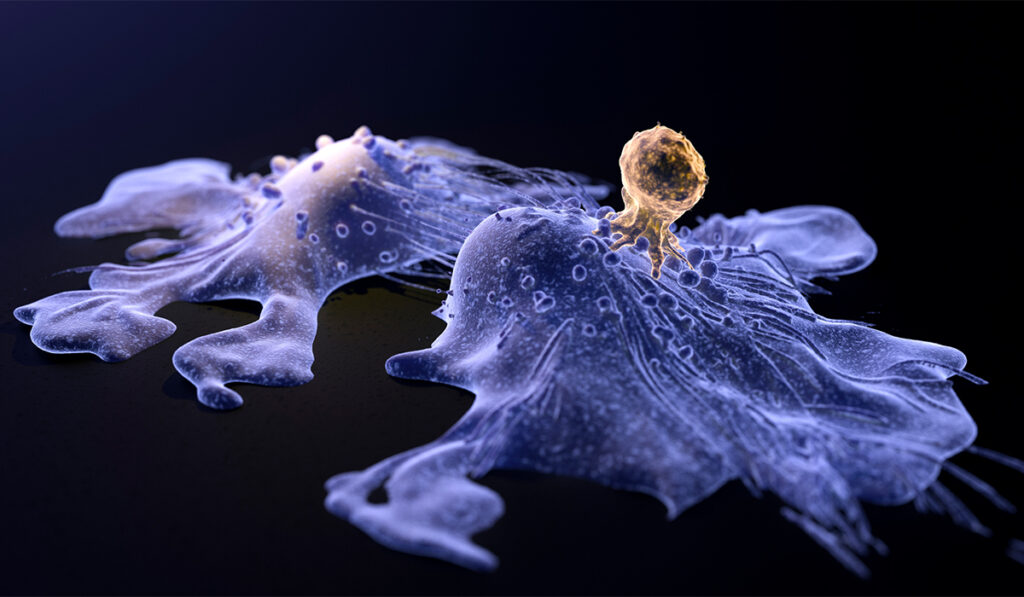
In people with cancer, tumor-specific CD8+ T cells become dysfunctional, or too “exhausted” to carry out their role in destroying malignant cells, leaving them to proliferate.
While it’s been thought that these immune cells creep into a state of exhaustion between days and weeks after encountering a tumor, recent research from cancer specialist Mary Philip, M.D., Ph.D., reveals that CD8+ T cell exhaustion occurs much more quickly – within a matter of hours.
The surprising findings, published in Nature Immunology, challenge previous ideas about how and why cells become exhausted, said Philip, an assistant professor of medicine in the division of hematology and oncology at Vanderbilt University Medical Center.
“I don’t think anyone expected that within six to 12 hours, T cells would look dysfunctional or exhausted; that’s a very fast time window.”
“The idea has been that T cells that are exposed to an antigen for a long time are working and working, and then at some point they sort of peter out. That’s where the term exhaustion comes from,” Philip said.
“I don’t think anyone expected that within six to 12 hours, T cells would look dysfunctional or exhausted; that’s a very fast time window.”
To explore how tumor-activated T cells become exhausted, as well as identify targets that could prevent or reverse that change in status, Philip and her colleagues used their previously established genetic mouse model of liver cancer. The researchers introduced trackable T cells into the model and then studied how the cells responded to established tumors.
The researchers also conducted parallel studies to model an effective T cell response, tracking how the cells responded to acute infection. In the context of infection, Philip explains, T cells become functional, whereas in the context of tumors, they become dysfunctional.
“This comparison allows us to compare what a ‘good’ T cell looks like versus a dysfunctional T cell,” she explained.
Failing Fast
In earlier studies using these mouse models, published in 2016 and 2017, the researchers found that tumor-activated T cells were dysfunctional after only five days. Further gene expression analysis at this time point revealed thousands of differences between tumor-activated and infection-activated T cells.
In following up their earlier studies, the team was hoping to find fewer differences between infection-activated and tumor-activated T cells, potentially pointing the way to key genes or signaling pathways as potential targets for making the dysfunctional T cells “good” again.
Instead, they found all the hallmarks of T cell exhaustion within an abbreviated period of time – just six to 12 hours – as the cells experienced dramatic changes in chromatin accessibility and gene expression.
“We still have thousands of different genes yet to look at,” Philip said.
The researchers reported that T cells in a metastatic melanoma model also became dysfunctional within hours, demonstrating that the response is not dependent on tumor type.
Further studies showed that transferring a tumor’s dysfunctional T cells into tumor-free mice does not cause the T cells to regain function, suggesting that the changes are imprinted. Conversely, introducing fully activated T cells into tumor models causes them to become dysfunctional, showing that negative tumor signals can override the cell’s functional programs.
Giving T Cells a Boost
Despite not finding key targets in the gene-expression data, the researchers did uncover certain trends, such as increased expression of inflammation-associated genes and transcription factors during infection, which are not turned on in the tumor model. They are now exploring whether infection and other ways of activating innate immune pathways may boost T cell function against tumors.
The researchers have been able to use data from these and other studies to identify biomarkers that allow them to predict whether T cells will respond to a tumor or not, which could help personalize immunotherapies.
“We know that checkpoint inhibitors and other immunotherapy interventions don’t work in a lot of patients,” Philip said. “It’s important to be able to predict response and avoid therapies that won’t benefit patients.”
*A version of this story originally appeared in the VUMC Reporter.