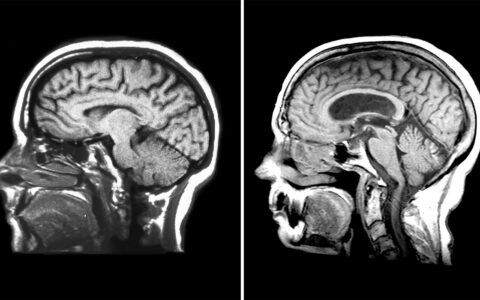
Hereditary transthyretin amyloidosis (ATTRv) is an autosomal dominant disease that causes peripheral neuropathy due to mutations in the transthyretin gene.
Transthyretin misfolding and aggregation is known to be associated with amyloid disease. If left untreated, it can lead to death within 10 years.
The most common ATTRv mutation in the United States, V142I, disproportionately affects African Americans. It has a primarily cardiac presentation, and knowledge of peripheral system involvement remains dim.
In a new study, researchers characterized and compared the V142I ATTRv mutation with other known ATTRv mutations to gain insight into peripheral involvement.
“We know that the V142I mutation causes cardiomyopathy,” said Amanda Peltier, M.D., division chief for the neuromuscular division at Vanderbilt University Medical Center and a principal investigator. “Our goal in this study was to determine how many of these patients also have peripheral neuropathy in addition to cardiac involvement.”
Because ATTRv has multiorgan involvement and great variability in clinical presentation, it represents a diagnostic challenge for neurologists, Peltier said.
“Presence of polyneuropathy may serve as a biomarker to help us detect ATTRv early and begin treatment with gene inhibitors. Without treatment, ATTRv is fatal.”
Evolution of Testing
Peltier began researching polyneuropathy during her training at the University of Michigan.
“We found a large number of prediabetic patients with peripheral neuropathies,” she explained. “We thought then that polyneuropathy might be an early manifestation of diabetic neuropathy.”
At the time, there weren’t a lot of good ways to measure small fiber neuropathies because they didn’t show up in nerve-connection tests performed in the electromyography (EMG) lab, Peltier said.
“EMGs are great for large fiber neuropathies, and we were also exploring autonomic testing like QSART [quantitative sudomotor axon reflex test] for those,” she said.
“Our primary interest was in how we identify these small fiber neuropathies and treat them early. This was where I first learned about punch skin biopsies.”
In small fiber neuropathies, skin biopsy can be a more sensitive measure for examining abnormalities in the target nerves, namely unmyelinated axons carrying pain sensation. It also allows small fibers with different functions to be investigated separately.
“Because the nerve involvement is highly variable, biopsy allows you to do multiple punches – the ankle, knee, and sometimes, the hip.”
Polyneuropathy and ATTRv
The ATTRv study team retrospectively measured the presence of polyneuropathy in both V142I and non-V142I carriers. Neurological, autonomic, and cardiac symptoms, as well as electrodiagnostic study results, were reviewed for each patient.
“The test is readily available; the question is when do you administer it?”
Approximately three-quarters of V142I carriers had signs of polyneuropathy, with abnormal pinprick sensation and temperature loss, weakness, and some loss of deep tendon reflexes. In some patients, presence of lightheadedness and gastrointestinal symptoms suggested autonomic involvement.
“Some of our patients were described with polyneuropathy before they had any cardiopathy,” Peltier noted. “The test is readily available; the question is when do you administer it?”
Polyneuropathy often manifests first as carpal tunnel syndrome in people who perform repetitive work with their hands. In the study, polyneuropathy characteristics and prevalence of carpal tunnel syndrome did not differ significantly between V142I and non-V142I carriers.
Peltier recommends that anyone who presents with carpal tunnel or pain in their tendons and ligaments – especially African Americans – be tested for ATTRv.
“Ultimately, we hope to identify the threshold at which these cases should be referred for neurological testing,” she said.
Expanding Detection and Treatment
Peltier and colleagues have been at the forefront of drug development for polyneuropathy treatments, including patisiran and topiramate. They are currently conducting skin biopsies to study myelinated nerve fibers in patients with early chronic inflammatory demyelinating polyneuropathy.
“We hope to determine if we can better detect demyelination as well as specific information about remyelination during treatment with IVIG [intravenous immunoglobulin],” she said.
The researchers also developed a shortened survey of autonomic symptoms in amyloid patients, and plan to do a follow up study validating it against the COMPASS 31 evaluation tool.
“The advantage would be to use this in cardiology offices, where they may not have a knowledgeable neurologist to help them recognize patients with neuropathy,” Peltier said.