In a coma with high intracranial pressures, most experts would have given 6-year-old Marcie a needle-thin chance of survival following her hemicraniectomy.
Yet, in the pediatric ICU (PICU) at Monroe Carell Jr. Children’s Hospital at Vanderbilt, a series of what-ifs led to a vortex of intense efforts that turned what seemed an impossible task into modern-day miracle.
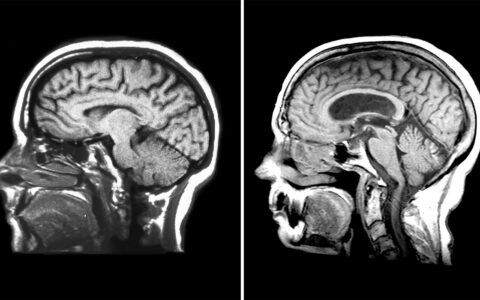
Born with five congenital heart defects requiring surgery, including a shunt placed between her right ventricle and pulmonary artery, Marcie was no stranger to pediatric intensive care. In December 2022, she had another surgery to replace the shunt with a larger one. Subsequently, she suffered an infarction in the part of her brain served by the left anterior and middle cerebral arteries, and swelling began to compress various regions of her brain.
An emergency CT scan uncovered evidence of uncal and tonsillar herniation. Concerned that the swelling would irrevocably damage her brain, pediatric neurosurgeon John (Jay) Wellons, M.D., M.S.P.H., conducted a left hemicraniectomy.
Prospects Dim Further
Katharine Boyle, M.D., a pediatric intensivist, began to oversee Marcie’s care following surgery. With continued high pressure on her brain, the PICU team decided to induce a coma.
The goal was to lower cerebral-perfusion pressure, the intracranial pressure and metabolic rate, regulate blood pressure and CO2 levels, and maintain oxygen saturation above 92 percent.
Still, her intracranial pressures hovered around 30 mmHG, with spikes as high as 50 (10-30 mmHG over the threshold of 20).
Boyle: Because we are one of the highest-volume PICUs in the Southeast, we are very well-prepared to handle the most difficult cases. But because we treat so much trauma, when we see someone who has such a slim chance of surviving, as we work we often ask ourselves, ‘Why are we putting them through this?’ And Marcie’s case was no exception.
48-Hour Full-Court Press
Wellons then assembled the PICU team to redefine the game plan. Entreating the team to suspend disbelief about the child’s long odds, he recommended what he termed a “full-court press” for 48 hours to bring Marcie out of her downward spiral.
I thought we needed to take a pause from the high emotion of this case and just focus on what we could do in those two days.
Wellons: We’re human, and sometimes you can get caught up in how sad the situation is and how we should handle communications with the parents and the wishes of the parents – all those delicate issues. I thought we needed to take a pause from the high emotion of this case, where we saw this little girl going from a good prognosis after cardiac surgery to spiraling downward and just focus on what we could do in those two days.

They concentrated their efforts on Vanderbilt’s rigid pediatric traumatic brain injury protocol, with two-to-three nurses at her bedside around the clock managing drips and tubes and EEG wires, and vigilantly monitoring and responding to vital sign changes.
When the 48-hour period ended, the team lightened sedation. Expecting a 48- to 72-hour tapering period before Marcie began easing out of the coma. Boyle was surprised to see the 6-year-old move her left leg within 24 hours. Soon after, she opened her eyes. Recovery was underway.
When she left the hospital 25 days later, Marcie was not yet walking or to able to eat by mouth, but she was making steady progress. Today, she is walking, running and roller skating.
I think we are all more inclined to expect and work even more relentlessly for our patients’ recovery.
Of course, she wore a helmet until her skull was surgically repaired in spring 2023 and is still relearning some communication skills, but the odds of a full and rewarding life are in her favor.
Boyle: In the end, our team, Marcie, and her parents, who were remarkable partners in this, had defied the most daunting odds. As a result, I think we are all more inclined to expect and work even more relentlessly for our patients’ recovery.