Researchers at Monroe Carell Jr. Children’s Hospital at Vanderbilt conducted a follow-up study to the multi-center Management of Myelomeningocele Study (MOMS) trials that found equivalent outcomes between the bipedicle flap technique and conventional closure for the neural tube defect.
The follow-up study based on the researchers’ own experiences was led by primary investigator and plastic surgeon Stephane Braun, M.D., chief of pediatric neurological surgery John (Jay) Wellons, M.D., and director of maternal fetal medicine Kelly A. Bennett, M.D.
MOMS Mission
The central mission of MOMS was to compare outcomes of pre- and postnatal closure of myelomeningocele, the most serious form of spina bifida. Numerous physician-researchers at Monroe Carell contributed to the MOMS trial and have conducted additional studies on treatment of myelomeningocele to further improve outcomes.
Those results have shown that performing fetal surgery is superior to postnatal surgery, resulting in a reduced need for CSF shunting, fewer revision surgeries, and improved mobility and independent functioning. This, in large part, was seen as capitalizing on a window of opportunity to reverse some of the factors that cause Chiari II malformation.
“They actually halted the MOMS trial early after looking at the outcomes from the enrolled patients who had come back in for follow up. The benefit to prenatal repair was so strong that it became unethical to continue the trial,” Wellons said. “Since then, we have been looking at specific aspects of the procedure to further guide surgeons and improve the prospects for these babies.”
A remarkable 161 of the original 183 mother-baby pairs have participated in decade-long follow-up, Wellons said, providing the opportunity to study functional outcomes throughout youth.
Bipedicle Flap Study
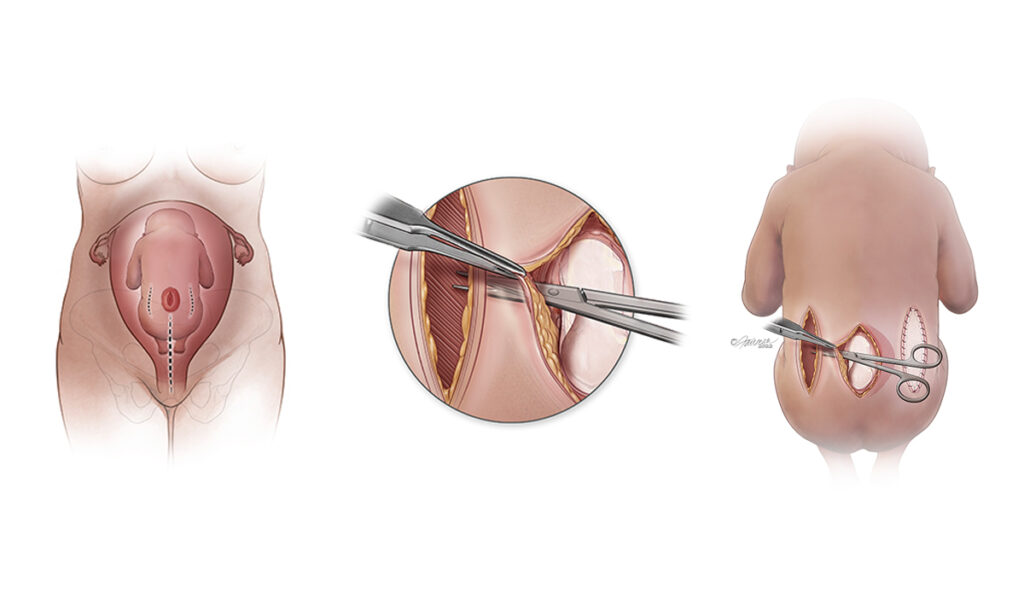
In the Vanderbilt team’s most recent research, they compared data on a new cohort of 86 patients who underwent fetal myelomeningocele repair at Vanderbilt between 2011 to 2021, comparing lineal and bipedicle closure. The latter included those with wide lesions previously not considered reparable via fetal surgery.
“This finding should expand inclusion criteria for fetal repair.”
“There is considerable stretching required to suture large high-tension lesions with straight linear repair,” Wellons said. “We wanted to know if bipedicle flaps, using acellular dermal matrix to fill the two relaxing incisions in the fetus’ sides, would enable a more durable suture of the central lesion over the spinal canal.”
“We found good outcomes with this thicker and healthier skin layer covering the open defect. This finding should expand inclusion criteria for fetal repair to fetuses with wider lesions.”
They looked for differences in the mothers’ health, as well as rates of fetal morbidity and mortality, midline repair site dehiscence, and the need for cerebral spinal fluid diversion. There were similar results between the two groups.
“Because the bipedicle flap technique stretches less of the skin in high-tension lesions, it also puts less stress on the midline scar.”
“Because the bipedicle flap technique stretches less of the skin in high-tension lesions, it also puts less stress on the midline scar,” Wellons said. “We found the mean duration of surgery is longer, which makes sense because it is a more complex surgery. In spite of this, there were no significant differences in long-term functional outcomes, which is exactly what we had hoped to find.”
Related Study Highlights
MOMS analyses address concerns around the slightly shorter gestational period and greater maternal and fetal complications evident in these procedures. While the potential benefits are compelling, the researchers have been especially attuned to any gap between cohorts.
Led by Bennett, a follow-up analysis showed reduction in the risk of premature membrane rupture, chorioamnionic separation and preterm delivery when surgical teams ensured that the uterine lining was included in the sutures placed when opening the uterus.
Another Vanderbilt study allayed concerns that intrauterine repair might require more detethering – a separation of the spinal cord from the canal. The need to detether was found to be equivalent regardless of whether surgeons used intrauterine or postnatal myelomeningocele repair techniques.
Sharing the Know-How
Over the last decade, Wellons has presented over 30 lectures across the country, sharing MOMS data and training neurosurgeons at several centers in how to perform the prenatal repair procedure, including the bipedicle flap approach.
“We are fortunate to have a large group here at Monroe Carell who share a firm mindset of wanting to continue to study and hone this procedure to provide the very best care of these babies and their mothers,” Wellons said. “We have the advantage of 20 years of MOMS outcomes data to guide us in this path.”