Single-center trials have demonstrated improvements in survival and fewer systemic side effects with hepatic artery infusion pump (HAIP) chemotherapy in patients with colorectal cancer that has metastasized to the liver.
However, use of the HAIP has been slow to spread beyond the doors of a handful of academic medical centers, in part due to the absence of a large multicenter trial. Now, such a study has been funded with Vanderbilt as a participating site.
“The pump gives patients who have failed systemic chemotherapy the opportunity for a longer life and, more importantly, improved quality of life.”
“This trial, now in the planning stages, should tell us whether HAIP chemotherapy, in addition to systemic chemotherapy, is superior to systemic chemotherapy alone in improving survival and quality of life in patients with unresectable colorectal liver metastases,” said Sekhar Padmanabhan, M.D., the surgical oncologist who launched the HAIP program at Vanderbilt University Medical Center.
According to Padmanabhan, existing experience has shown that the pump gives “patients who have failed systemic chemotherapy and have few remaining treatment options the opportunity for a longer life and, more importantly, improved quality of life,”
Direct Delivery Supercharged

While the pumps designed for patients who are not good candidates for surgery, those with resectable disease, or disease that cannot be completely removed with surgery, may also benefit from HAIP chemotherapy, he said.
About 25 to 30 percent of patients diagnosed with colon cancer eventually develop liver metastases. Liver resection is the only potentially curative treatment, but 70 to 80 percent of patients will have recurrences, typically in the liver or lungs.
“Historically, once patients have developed metastatic disease to the liver they have been treated solely with systemic chemotherapy,” Padmanabhan said. “But in the absence of any surgical resection, these patients haven’t lived longer than five years. What we’ve learned in the last 20 to 30 years is that if you can resect the metastatic liver disease, those patients will live longer.”
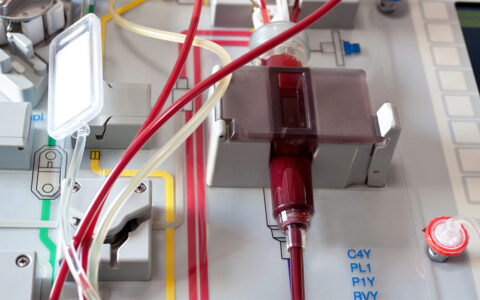
The HAIP is a promising candidate, Padmanabhan says, because it delivers up to 400 times the dose of chemotherapy that can be safely delivered systemically.
This can help reduce liver recurrence, prolong survival in patients with unresectable disease, and convert unresectable tumors into resectable ones. While it is currently indicated for use in colorectal liver metastases, it has also been shown to be effective in patients with intrahepatic cholangiocarcinoma that cannot be surgically removed.
Treatment Protocol
Implanting the pump is safe and relatively uncomplicated in experienced hands, Padmanabhan says. The hockey puck-sized device rests on top of the abdominal muscle wall. Chemotherapy is injected into the pump, which uses body heat to slowly infuse the drug into the liver via the hepatic artery. In this way, the drug is primarily metabolized by the liver, sparing other organs and tissues.
The protocol typically calls for two weeks of chemotherapy, followed by two weeks off, to allow the liver to rest. This continues for as long as required, barring liver toxicity. In the meantime, oncologists are watching and waiting.
“The goal is to shrink an uresectable tumor so that it can be resected or to prevent a liver recurrence in patients we have resected, so we’re constantly reassessing the patient through imaging – mostly CT scans – to see if we have reached that point,” Padmanabhan said.
Defining HAIP Indications
With large medical centers like VUMC able to offer this therapy now, Padmanabhan says the time is ripe for the clinical trial, which will help surgical oncologists determine, one way or the other, whether they should continue using the pump – or focus elsewhere.
“Phase 2 clinical data suggests that about half of patients who present with initially unresectable disease can convert to resectable disease with this therapy,” Padmanabhan said. “But the modern systemic chemotherapy drugs – like oxaliplatin, irinotecan, bevacizumab, and cetuximab –
have never been compared with HAIP and its delivery of floxuridine. We’re basically using it now because we are finding that it works better. To know it works better, though, we need to formally test it.”
“About half of patients who present with initially unresectable disease can convert to resectable disease with this therapy.”
Finding best therapies will be increasingly important as the incidence of colorectal cancer continues to rise. Already, it has become the second most common cause of cancer-related mortality in the United States, and incidence is rapidly increasing in people under age 50.
Padmanabhan urges early referral of patients with colorectal liver metastases to hepatobiliary surgical oncologists.
“There are many patients out there on palliative chemotherapy who could be evaluated for potential tumor resection and HAIP chemotherapy,” he said.