Endometrial ablation has helped women over the past several decades find relief from uncontrolled menorrhagia. Yet, the procedure is not without its risks, including pain and risk of scarring within the uterus.
In 2019, Howard Curlin, M.D., a minimally invasive gynecological surgery specialist at Vanderbilt University Medical Center, was site co-investigator testing the Cerene device, developed by Channel Medsystems for in-office cryotherapy ablation. The device was approved by the FDA after demonstrating its utility in the multicenter, prospective CLARITY trial.
“It offers greater assurance of cavity access if future examinations and procedures are needed.”
Hallmarks of the three-phase study include high participant retention rates that enabled results from 12- and 36-month follow-up contacts. Twelve-month results published in the Journal of Minimally Invasive Gynecology showed that the Cerene device was safe and relatively painless for patients, plus more user-friendly and efficient for practitioners than traditional ablation.
“I think its use will increase in patients seeking endometrial ablation because of its efficacy and how well-tolerated it is as an in-office procedure,” Curlin said, adding that the technique also helps avoid the risk of uterine scarring. “It offers greater assurance of cavity access if future examinations and procedures are needed.”
Menorrhagia is Common
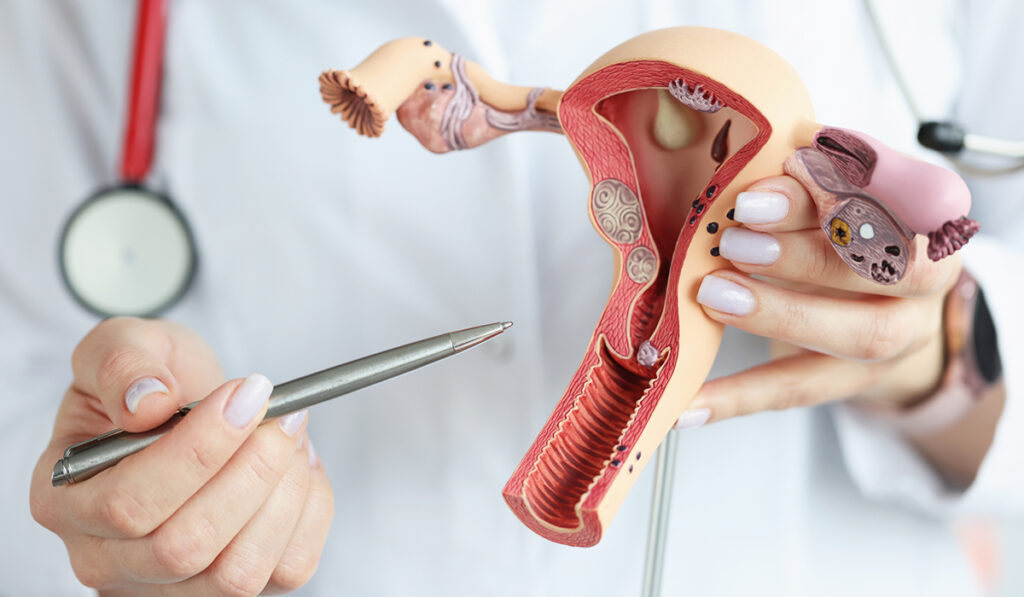
Curlin says one out of every five women experiences serious heavy menstrual flow, usually accompanied by severe cramping and other side effects. Heavy bleeding can stem from structural causes, including fibroids, polyps and myomas. However, a large proportion of women experience menorrhagia for non-structural, hormonal or idiopathic reasons. For most of these women, he says non-resectoscopic endometrial ablation is an option and may obviate the need for hysterectomy.
First-line treatment of menorrhagia is oral or IUD hormonal therapy, but Curlin says many women do not want to pursue this treatment while others fail medicinal therapy. For them, endometrial ablation, with its more than 90 percent success rate, offers a second or alternative opportunity for relief.
Drawbacks of RF Ablation
For these women, radiofrequency (RF) ablation has been the predominant modality. RF ablation sends high frequency waves through a device, using the body as part of the circuitry to heat and destroy cells.
Risks include unintended thermal effects, and typically moderate pain that requires anesthesia and pain medications. Most concerning, Curlin said, are the bands of fibrous scarring or adhesions that are a frequent byproduct of RF ablation.
The scarring is major drawback, frequently becoming an impediment to accessing the uterine cavity after treatment. If heavy bleeding should return, the lack of access could preclude evaluation of serious developments, like precancerous changes. He says these situations often dictate that a hysterectomy be performed or, at the least, while limiting future use of an IUD.
The Cryotherapy Alternative
Curlin says about 75 percent of ablations are done via RF, and others with a variety of techniques, including heated hysteroscopic fluid, water vapor and cryoblation.
The Cerene device requires insertion of the tip of the instrument into the uterus until it abuts the fundus, where it is positioned to emit nitrous oxide into the thin uterine lining. Ice crystals conform to the lining, ablating the endometrium.
“It is a win in terms of cost-savings and, importantly, cavity access is almost universally maintained.”
This rapid freezing is followed by rapid thawing, which causes cell membrane rupture and cellular dehydration, and induces vascular changes that result in tissue ischemia. Treatment with cold gas has an analgesic effect, Curlin emphasizes, so there is generally no need for sedation and only local anesthetic.
“The minimization of pain was one of the things that impressed me most when we did the study and saw how well patients tolerate it in the office,” Curlin said.
“That, and the fact that the procedure is only two-and-a-half minutes long once the device is in place. It is a win in terms of cost-savings and, importantly, cavity access is almost universally maintained.”
CLARITY Makes the Case
The CLARITY study included 242 women between the ages of 25 and 50 years who underwent cryoablation. Nearly 90 percent participated in the 12-month and 36-month follow-up sessions.
The cryoablations were primarily performed as an in-office procedure, with only 3 percent of patients requiring intravenous sedation, and none requiring general anesthesia. The median reported pain rating was below two, on a one-to-10 scale.
Twelve months later, the participants’ self-scored mean measure of bleeding volume dropped by a factor of seven. When asked to describe their last menstrual period, over 90 percent reported that they no longer were having a period or were having normal or lighter-than-normal menstruation. Over 95 percent rated their improvement as meaningful, and 90 percent said they were satisfied or very satisfied with the outcomes.
At 36 months, the follow-up results were nearly identical, demonstrating durability of the results.
Beyond Menorrhagia Treatment
Cryotherapy has previously been used in dermatology, and its uses are growing in other areas, such as cardiac ablation, lung nodule ablation, and treatment of treatment of renal lesions, hepatic lesions and gynecologic fibroids.
“The same advantages of an improved pain profile and lower collateral damage apply in other procedures,” Curlin said. “I expect cryotherapy to continue to gain momentum.”