Neurologists treating refractory focal seizure patients report encouraging results from a trial of cenobamate, with results showing full-time seizure relief achieved over 12 months by about 30 percent of this hard-to-treat group.
Cenobamate, a dual sodium channel blocker and gamma-aminobutyric acid (GABA) enhancer, was put to the test in a phase 3 trial that included up to 43 months of open-label study. The drug is now FDA-approved for use in focal seizures in adults.
“Cenobamate may be considered early in the treatment regimen.”
Vanderbilt University Medical Center neurologist Bassel M. Abou-Khalil, M.D., who served as principal investigator, presented a post-hoc analysis of the trial at the 2022 American Academy of Neurology conference. The analysis compared clinical outcomes of open-label adjunctive cenobamate treatment between patients with drug-resistant epilepsy who had prior surgery or neurostimulation, and those who did not.
“Trials provided evidence that cenobamate rendered about a third of refractory patients seizure-free overall and was well-tolerated,” Abou-Khalil said. “This analysis suggests that cenobamate may be considered early in the treatment regimen and, particularly, as an option for patients who are not good surgical candidates.”
Quest for Medications
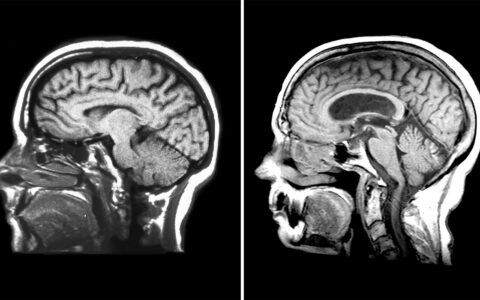
Focal seizures originate from specific sites in the brain, and may have a combination of motor, sensory, autonomic or psychic manifestations.
People experiencing focal seizures “may have preserved awareness or partially impaired awareness, but may also have complete loss of awareness and may evolve to bilateral tonic-clonic activity,” Abou-Khalil said. Even when there is incomplete loss of awareness, he notes focal seizures can be temporarily debilitating.
Anti-seizure medications have a variety of mechanisms of action, most commonly blocking sodium channels and enhancing GABA, but cenobamate has both properties.
“We’ve tested many, many drugs in people with drug-resistant focal epilepsy,” Abou-Khalil said. “Most of these individuals have failed multiple medications and some have even failed surgery. Only about 30 to 50 percent of patients have their seizures cut in half or better through these drugs, and fewer than 8 percent are seizure-free.”
Drug Efficacy After Failed Surgery
Patients who have failed epilepsy surgery are a particularly drug-resistant group. One study conducted before cenobamate marketing found that after failed surgery, only 9.7 percent of patients attained seizure freedom with medication additions or adjustments.
“Other studies have shown similarly disappointing success rates when combining and adjusting various anti-seizure medications post-surgery,” Abou-Khalil said.
Abou-Khalil’s post-hoc analysis was the first to stratify surgical and nonsurgical patients with uncontrolled seizures and examine the efficacy of cenobamate in each group.
Disparate Benefits
The analysis looked at 240 patients who had uncontrolled focal seizures despite treatment with 1-3 concomitant anti-seizure medications at stable doses. All patients added cenobamate to their regimens. The median duration of cenobamate exposure was 30.2 months.
The surgical patients in the study (35.4 percent) had undergone resection, corpus callosotomy, tumor removal, ablation, vagus nerve stimulation or responsive neurostimulation. This highly treatment-resistant group had about double the focal seizure rate at baseline than the non-surgical group and were more likely to be on three or more medications.
Complete seizure freedom in any consecutive 12-month interval occurred in 30.6 percent of those who had had prior surgery, and 39.4 percent of nonsurgical patients.
“The seizure-free rate of post-surgical patients is exceptional.”
Among the 177 patients still receiving cenobamate at data cutoff, 29.2 percent of surgical and 36.6 percent of nonsurgical patients were seizure free for at least 12 months.
“While nonsurgical patients derived greater benefit, the seizure-free rate of post-surgical patients is exceptional,” Abou-Khalil said.
Cenobamate Plus Clobazam
Additional support for cenobamate came in 2023, when Abou-Khalil and Vanderbilt research nurse specialist Melissa Osborn, R.N., published a study looking at potential synergy between cenobamate and clobazam. They found that low-dose clobazam may further raise seizure-free rates in patients who have an incomplete response to cenobamate.
“These patients had also failed to respond to clobazam without cenobamate,” Abou-Khalil said.
Clobazam, also a GABA enhancer, is FDA-approved for the treatment of seizures associated with Lennox-Gastaut syndrome in children and adults, but it is also used to treat focal seizures.
Cenobamate has a known pharmacokinetic interaction with clobazam, Abou-Khalil explained.
“Cenobamate causes accumulation of the active byproduct of clobazam, such that the dose of clobazam has to be reduced upon introduction of cenobamate.”
“The best approach for a patient already on clobazam is to reduce the dose when starting cenobamate, rather than taking clobazam away. In patients still having seizures on cenobamate in the absence of clobazam, consider adding a very small dose of clobazam,” Abou-Khalil said.