Bronchopulmonary dysplasia (BPD) is the most common complication of preterm birth, severely affecting about 50 percent of infants born earlier than 28 weeks’ gestation, says Jennifer Sucre, M.D., a pediatric neonatologist at Monroe Carell Jr. Children’s Hospital at Vanderbilt.
While many of the environmental exposures associated with BPD are well-described – including premature birth, inflammation, and prolonged mechanical ventilation –few tools exist that can identify which infants are most at risk.
To address this knowledge gap, researchers at Monroe Carell leveraged a NICU clinical registry database and existing EHR data to identify maternal and antenatal risk factors for developing BPD in the setting of preterm delivery.
Sucre was the principal investigator on this research, in collaboration with data scientist Lisa Bastarache, M.S., and first author Meredith Campbell, M.D., a neonatology fellow, both of Vanderbilt. They catalogued 20 prenatal exposures and their relative association with BPD risks, reporting their findings in Pediatric Research in 2022.
“Of the exposures studied, preterm polyhydramnios was most significantly associated with BPD.”
“Of the exposures studied, preterm polyhydramnios was most significantly associated with BPD,” Sucre said. “While these are preliminary associations, we are hoping that neonatologists can use this knowledge to help inform clinical risk for BPD in preterm infants.”
In Utero Associations
Monroe Carell’s NICU registry, built under the leadership of Steven Steele, R.N., includes 4,527 infants born between 22- and 34-weeks’ gestation from 2005 to 2017. The cohort is comprised of 1,385 BPD cases and 3,142 infants without BPD. It includes 280 clinical features for each patient.
For the study, the team combined this registry with a large EHR dataset and performed a phenome-wide association study (PheWAS) using a technique pioneered at Vanderbilt.
They interrogated associations between BPD and antenatal exposures and maternal health factors, confirming known significant associations with BPD, such as low gestational age, low birth weight, and male sex. Consistent with prior studies, there was no association found for antenatal steroid use in BPD prevention.
A Novel Finding
What they learned about in utero associations, however, was novel: an excess of amniotic fluid in the womb was a top risk factor.
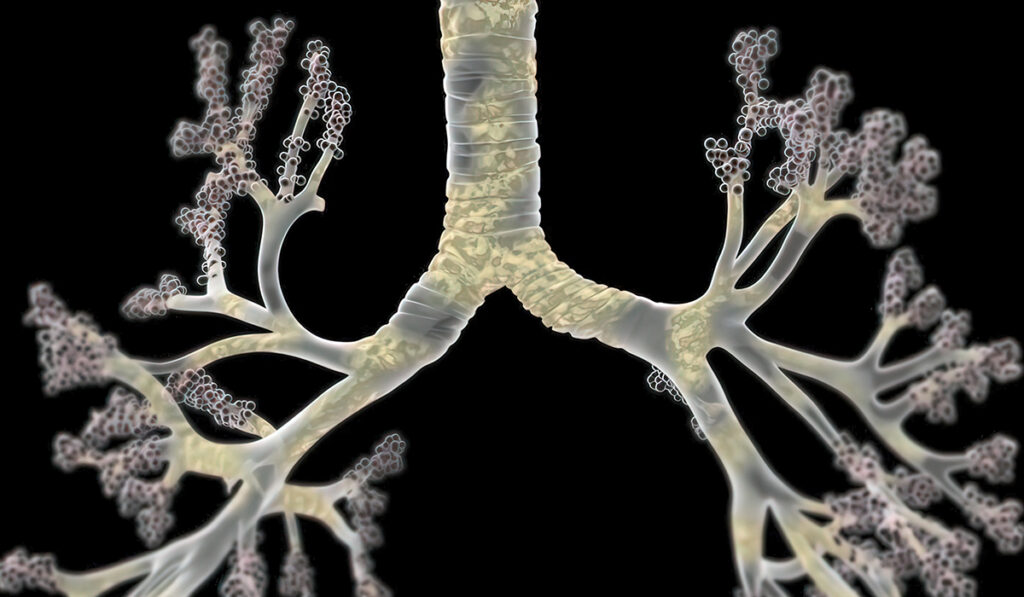
Low levels of lung fluid and prolonged membrane rupture have been associated with pulmonary hypoplasia in both animals and humans. However, the relationship between excess amniotic fluid and abnormal lung development has received less attention. The findings surrounding polyhydramnios suggest new hypotheses about its impact.
Sucre says infections can result from polyhydramnios, and development of polyhydramnios in the second trimester – unlike third trimester polyhydramnios, which is associated with diabetes and birth defects – may be a clinical indicator of early placental inflammation.
“It is also possible that the hydrostatic pressure from excess amniotic fluid alone results in primary lung injury,” she said. “This increased pressure may decrease alveolar epithelial differentiation and lung maturation, predisposing infants to worsening respiratory distress at birth and BPD.”
Treatment Modification
Sucre says probing the content of the amniotic fluid in infants with second-trimester polyhydramnios and investigating associations with placental pathology will help characterize causal relationships.
Such follow-up studies are planned, using a more granular stratification of BPD staging by degree of respiratory support.
“We hypothesize that preterm polyhydramnios may be a clinical indicator of placental inflammation, even in the absence of obvious infection, and that it could be used to identify which infants are at the highest risk of developing BPD after preterm birth,” Sucre said.