Discoveries in Medicine presents a three-part interview with innovator William H. Fissell, M.D., a nephrologist who is managing the development of the first implantable biohybrid artificial kidney, from concept through production.
Link to Part I: The Implantable Biohybrid Artificial Kidney (iBAK): Part 1: From Concept to Preclinical Trials.
Discoveries in Medicine: Dr. Fissell, we talked last time about the motivation behind iBAK’s development and the ease of implantation and cartridge replacement. Let’s dig into the nuts and bolts of this device. What are the bioengineering building blocks for the iBAK?
Fissell: Our bioengineering approach has simplified the problem down a single essential task: concentrating wastes from blood into urine. Kidneys have to remove all the wastes that your body’s cells produce every day, but at the same time, these chemicals cannot be allowed to build up to high concentrations in blood. Kidneys constantly scavenge dilute wastes from blood and concentrate them into a few liters of urine. We decided to copy the kidney’s approach of filtering blood and then concentrating the filtered fluid.
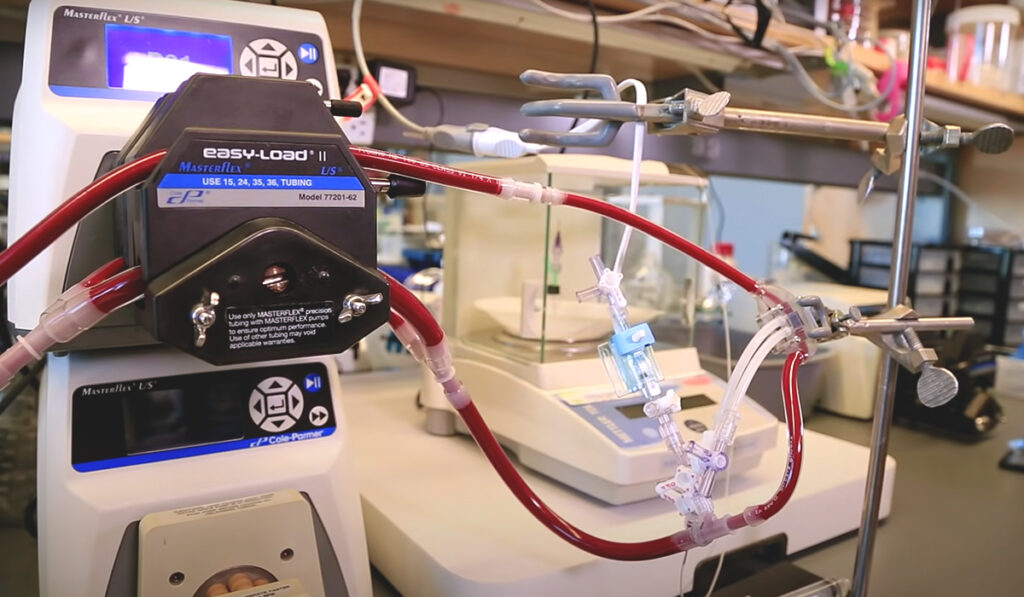
We didn’t want to rely on connections to pumps or batteries outside the body, and we didn’t want disposable sorbents or dialysate – we want people to be able to be people, not patients, so it has to work like a kidney. We invented a new membrane that is so efficient we don’t need electric motor pumps or batteries or drivelines — we just use the person’s blood pressure like the kidney does. Instead of using sorbents or charcoal or resins to concentrate wastes, we use the chemical energy of tubule cells — again, just like the kidney does.
Discoveries in Medicine: Would you describe how the iBAK filters blood?
Fissell: The surgeon sews a short length of graft material – like a hollow fabric tube – to an artery that carries blood to the filter we designed. The blood washes over a series of filters that are shaped kind of like storm drains, but 100 million times smaller. They keep the “good stuff” like red blood cells and antibodies in your blood, but they allow some of the salty water that makes up blood to go through the pores. Over the course of a day this adds up to a few gallons of salt water.
Even though that water has the wastes we want to get rid of, we can’t afford to get rid of all that water — we’d dry out. So, both the blood leaving the filter and the water leaving the filter are piped to a bioreactor of living kidney cells. There, the cells pump salt and water back to the blood, but block wastes from being reabsorbed with the water.
Ultimately, about nine-tenths of the fluid volume is reabsorbed and the wastes are concentrated tenfold into what we call urine!
Medical Management of Patients
Discoveries in Medicine: You mentioned that iBAK recipients would need medical management to maintain kidney function. What gap remains to be filled?
Fissell: A healthy natural kidney performs about 12 homeostatic functions for you. These include electrolyte regulation, blood pressure control, the synthesis of erythropoietin to stimulate your bone marrow to make red blood cells — a wide variety of functions. These are performed in the loop of Henle, the distal convoluted tubule, and the collecting ducts, which are not the central kidney functions iBAK replaces.
We worked to mimic a natural filtration rate that was likely to balance dietary intake of the minerals that are most troublesome in renal disease: potassium, phosphorus, calcium, and nitrogen. The operating point of the iBAK is between 15-30 ml/minute, which may mitigate some of the challenges of electrolyte and mineral balance. All the other kidney functions will be manageable through pharmaceutical therapy.
It’s not going to be completely hassle-free, but the patient who chooses an iBAK over dialysis will be healthy because the iBAK directly addresses the major causes of illness in dialyzed renal failure: the roller coaster ride of fluid accumulation and removal, which injures the heart, and the need for a severely restricted diet, which starves the patient.
Clearing the Bar
Discoveries in Medicine: What were the most challenging bioengineering hurdles in developing and perfecting the iBAK?
Fissell: We spent a decade on the filter. At times, we felt like Sisyphus pushing the same boulder the same distance every day. We were resource-limited, and to be honest, we faced some understandable skepticism. However, the vision prevailed, and we overcame the technical challenges by importing wisdom from a very wide range of disciplines, from computational fluid mechanics, to ceramics, to surface chemistry.
One of our biggest challenges was how to grow renal tubule cells that look and behave like they do in the body. Before I started this kind of work I had no idea that when you took cells out of the body and grew them in a dish, they deteriorated. I thought it was like a car: you park it and when you come out the next morning, it’s still a car — it didn’t morph into a tricycle overnight. But cells do change when they are in artificial culture, and they don’t function well.
We had our share of trial and error, but we actually learned that growing these cells on materials that were about as soft as healthy kidney tissue, instead of the hard plastic in a lab dish, allowed them to function much like cells in a healthy kidney. We went on to show that simple adjustments to cell culture protocols let kidney tubule cells reabsorb salt and water, block waste products, and excrete certain molecules just like healthy kidneys.
We had to learn how to power the device without external pumps and tubing. We did that by using blood pressure alone to power the filter.
Then, we had to answer the questions: will the host destroy the artificial kidney? Will there be an immune attack on the cells? Will there be clotting inside the membranes? Will our device supply enough oxygen and nutrients to the tubule cells we implant on the scaffold? Will it do the job of filtration and waste removal at the proper rate?
We have tackled and overcome each of these issues one by one over the past 20 years, and are encouraged by our preclinical studies. Our HemoCartridge and a BioCartridge of renal tubule cells have proven able to maintain viability and reabsorption function over 72 hours in vivo.
With sufficient funding, we are now ready to scale up for clinical trials in humans.