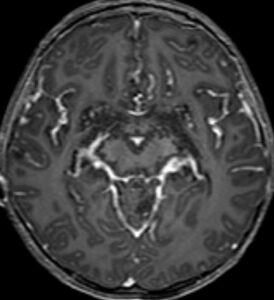
Pediatric low-grade gliomas are usually slow growing and unlikely to disseminate, in contrast to similar tumor types in adults. In rare cases, however, low-grade gliomas in children do spread, becoming aggressive and difficult to treat.
With $200,000 in funding from the Pediatric Brain Tumor Foundation, pediatric neurosurgeon Michael Dewan, M.D., will lead an international study to identify the molecular changes that trigger this malignant switch.
“This is by far the largest study that will specifically examine molecular alterations in disseminated low-grade glioma.”
“This is by far the largest study that will specifically examine molecular alterations in disseminated low-grade glioma,” said Dewan, who is working on the research with his colleagues at Monroe Carell Jr. Children’s Hospital at Vanderbilt and in close collaboration with the Hospital for Sick Children in Toronto, Canada.
An International Effort
The study aims to enroll about 200 pediatric patients with disseminated low-grade gliomas across more than 20 sites. Over a dozen sites are already up and running throughout North America, Europe, the Middle East, and South America, Dewan said.
“Disseminated low-grade gliomas are rare – in a year I might see three or four – and that is true of other high-volume centers like Vanderbilt,” Dewan said. “We recognize that we need many centers to contribute sufficient patients to achieve the kind of statistical power needed to draw actionable conclusions.”
Tissue from the gliomas will be shipped to a laboratory in Toronto where researchers will perform sequencing to better understand the molecular characteristics of the tumors. In some cases where the molecular data has already been obtained, the information can be submitted to a shared REDCap database.
All data generated from the cohort will be compared to a large databank of molecularly characterized nondisseminated low-grade gliomas maintained by Toronto’s Hospital for Sick Children.
Mutations of Interest
Already, Dewan and colleagues have assembled a list of alterations they suspect might promote metastases, including deletions or amplifications of chromosome 1p or 1q, BRAF alterations, CDKN2A deletion, mutations in TP53, IDH, or FGFR, and many others.
These early insights were uncovered through a recent literature review led by Dewan aimed at summarizing the genetic alterations and outcomes currently described for both disseminated pediatric low-grade gliomas and glioneuronal tumors. A total of 50 studies published between 1994 to 2020 were included in the review, representing a total of 366 cases.
Within cases of disseminated pediatric low-grade glioma specifically, 67 percent reported a chromosome 1p deletion, 42 percent a BRAF-KIAA 1549 fusion, and 10 percent a BRAF V600E mutation.
Additional molecular alterations of interest include those known to encourage metastases in other forms of cancer, Dewan said.
Global Impact
Results from the newly-funded study could accelerate the use of targeted therapies to prevent dissemination and improve survival outcomes.
“If we identify a molecular alteration associated with metastatic capability, we could potentially treat patients harboring that alteration with a targeted therapy upfront thereby reducing the risk of future tumor dissemination,” Dewan said. “This could take what would be otherwise a dubious five- or 10-year survival and put those patients on par with the other 90 percent that enjoy excellent survival after their diagnosis of low-grade glioma.”
“If we identify a molecular alteration associated with metastatic capability, we could potentially treat patients harboring that alteration with a targeted therapy upfront.”
An additional boon is the study’s inclusive design, which incorporates patients of varying socioeconomic status.
“I hope this will be the first of many studies that will incorporate researchers and patients from both high- and low-resource settings,” Dewan said. “This international collaboration demonstrates a rare, diverse symphony of investigators, neurosurgeons, oncologists and pathologists. The work we do together will have a direct impact on children here and around the world.”






