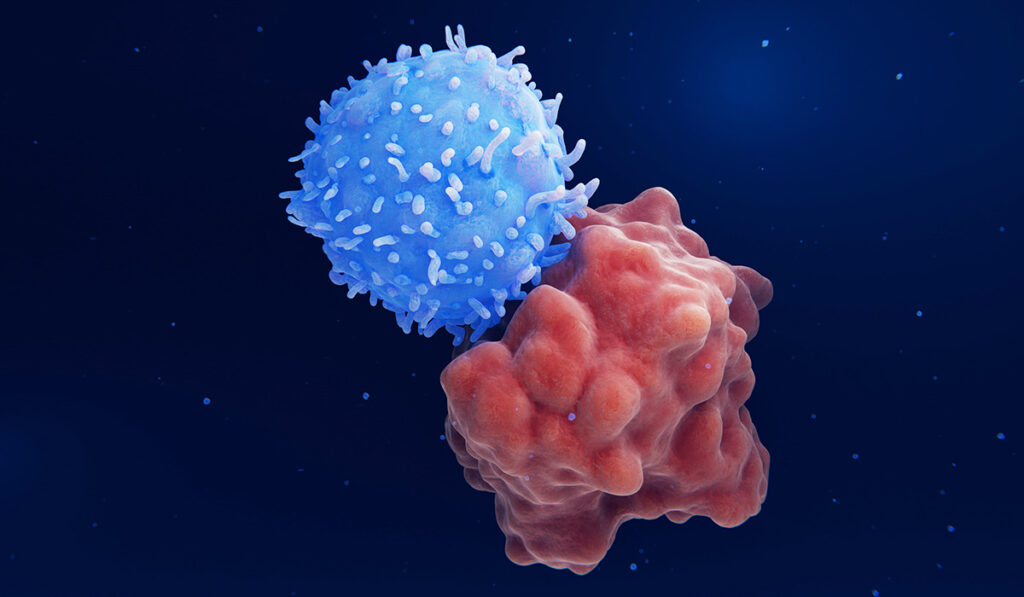
Chimeric antigen receptor (CAR) T-cell therapy has become a game changer for patients with aggressive large B-cell non-Hodgkin lymphoma (LBCL), offering hope to many and positive results for most, even patients with aggressive relapsed or refractory conditions.
Yet, the potential for serious neurotoxicity following therapy remains a significant drawback. Unlike traditional chemoimmunotherapy, CAR T-cell treatment triggers an intracellular reaction as the cells bind to their target, attracting an immune response to the site with adverse physiological side effects including fever, hypoxia and hypertension.
“It is clear that with CAR T-cell therapy have come unique toxicities,” said Vanderbilt University Medical Center oncologist Vivek Patel, M.D., a clinical fellow in the Department of Medicine.
Among the questions researchers have been asking are whether these reactions are somehow integral to the treatment process and whether strong or weak reactions could be used to predict a treatment’s effectiveness.
To investigate, Patel worked with another Vanderbilt fellow, Shakthi Baskar, M.D., and Vanderbilt assistant professor of medicine Olalekan O. Oluwole, M.D., to evaluate the risks and potential roles of cytokine release syndrome (CRS) and immune effector-associated neurotoxicity (ICANS) symptoms that are common in CAR T-cell-treated patients.
Datamining May Predict Risk
“Most people have it, although some don’t,” Oluwole said. “Those who have higher tumor bulk with more advanced disease tend to have more side effects.”
Earlier studies concluded that ICANS was associated with inferior overall survival in those who received T-cell therapy, but that was based on a small sample size, Patel said.
In their recent investigation, Patel’s team examined the histories and outcomes of 352 United States adults with LBCL who received axicabtagene ciloleucel (axi-cel) or tisagenlecleucel (tisa-cel) treatment between May 2018 and January 2021. The data were drawn from eight academic medical centers.
“In this multicenter retrospective study, we aimed to determine risk factors for ICANS and clinical outcomes in patients who develop ICANS,’’ said Patel, who presented at the American Society of Hematology® Annual Meeting and Exposition. The work was published in Blood Advances.
The researchers found neurotoxicity to be present in between 60 and 87 percent of patients following CAR T-cell therapy, Patel said. Approximately 75 percent of the study participants developed CRS. Slightly more than a third developed ICANS. Approximately 60 percent of patients who developed ICANS had cases considered “severe,” with the remainder of the cases labeled “mild.”
“After the infusion, developing CRS – and an earlier onset of CRS – were predictive of ICANS,” Patel said.
However, the investigators found no statistical difference in the rates of progression-free and overall survival between patients who had CRS and those who did not, and neither did severity of cases prove to be a factor.
“Patients who develop CRS have similar clinical outcomes compared to patients without CRS treated with commercial anti-CD19 CAR T-cells,” the report concludes.
Factors Beyond CRS
Higher-than-normal rates of lactate dehydrogenase (LDH) prior to chemotherapy were among factors tied to progression and survival.
“Bulky disease [≥10 cm], LDH greater than the upper limit of normal, and peak ferritin greater than 5,000 in the first 28-days post-infusion were associated with worse overall survival,” the authors wrote.
Previous studies have reported prolonged progression-free survival but also a higher toxicity for patients treated with axi-cel compared with tisa-cel. That finding was mirrored in Patel’s research retrospective. Among patients receiving axi-cel, 90.1 percent developed CRS, compared to 53 percent receiving tisa-cel.
“If someone has a high level of serum protein when given CAR [T-cell therapy], they should be monitored closely for neurobiological complications.”
Also of note was the finding that using steroids did not impact patient outcomes, providing support for continuing their use as a prophylactic or therapeutic measure.
“Future studies should identify novel predictive scores for ICANS which may lead to strategies to prevent neurologic toxicity after CAR T-cell therapy,” Patel said.
Oluwel agreed.
“The take-home message from this is that if someone has a high level of serum protein when given CAR [T-cell therapy], they should be monitored closely for neurobiological complications, and those should be addressed early before those side effects reach a higher grade,” he said.