Thoracic discectomy is a rare procedure that carries significantly greater morbidity than cervical or lumbar discectomy. The extent of bone removal and muscle dissection in traditional approaches to the thoracic spine can make the procedure high-risk and with a lengthy recovery, explained Raymond Gardocki, M.D., an orthopaedic surgeon at Vanderbilt University Medical Center
Gardocki is one of a select group of endoscopic spine surgeons working to expand the eligibility of patients for surgical relief. As someone who has run ahead of the pack for minimally-invasive surgery, he began performing endoscopic spine surgery seven years ago, and now performs awake, outpatient, endoscopic thoracic discectomies on patients from within and outside of the region.
“Thoracic herniations have been treated with a sort of benign neglect. But developments in endoscopic spine surgery have allowed us to change that,” Gardocki said. “We are able to go from a highly morbid surgery reserved for patients with significant neurologic deficits or very severe, intractable pain to one that is viable for patients who have less severe symptoms.”
“Thoracic herniations have been treated with a sort of benign neglect. But developments in endoscopic spine surgery have allowed us to change that.”
Instability and Collateral Damage
Gardocki said that with traditional surgical approaches to thoracic disc herniation, the cure may be worse than the disease.
“Patients with these herniations can have radicular pain around the chest, but if they don’t have significant neurologic findings, they are often told to wait it out, see if it gets worse, because the surgical approach is so invasive.”
The traditional approach, a thoracotomy, requires a thoracic surgeon to go through the chest and deflate the lung to get to the spine. The spine surgeon then removes a significant amount of bone anteriorly to access the spinal canal safely.
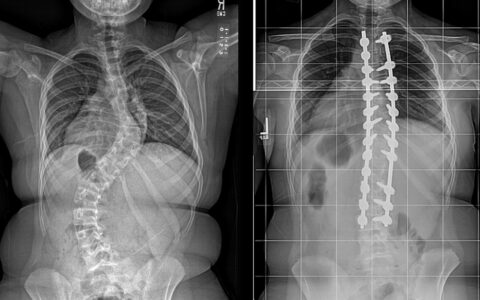
To avoid thoracotomy, surgeons may use an open trans-pedicular approach, Gardocki explains, where they come in from the back at a 30-45 degree angle. This avoids retraction of the spinal cord, but normally requires removal of a rib and pedicle, necessitating a posterior fusion with screws and rods.
“In all the posterior approaches, you cross multiple tissue planes and create instability by removing major structural components,” Gardocki said. “It’s a much more morbid procedure in thoracic than in cervical or lumbar discectomies.”
Even with a less invasive retropleural approach, the surgeon creates at least a 10-centimeter incision, removes a rib, and pushes the pleura down to gain access to the pathology. “This approach still requires removal of a rib and the pedicle, resulting in structural instability and fusion,” Gardocki said.
New Angle, Better Results
He contrasts these approaches to the optimized transforaminal endoscopic discectomy, which does not impart unnecessary iatrogenic trauma. The outpatient procedure requires no general anesthesia, has fewer complication risks, and leaves the patient with a short recovery time, minimal restrictions and no need for narcotics post-operatively, Gardocki said.
“When we remove the herniation with this procedure, we’re not causing iatrogenic instability because we don’t remove a rib or take down the entire pedicle,” he said. “We don’t need to do a fusion, which involves significantly more morbidity and expense.”
The surgeon directs a 7-millimeter cannula to the ventral spinal canal through the foramen to approach the resection.
“If you angulate the cannula, it allows safe access all the way across the midline of the spinal canal ventral to the spinal cord,” he said.
Because of the minimal tissue damage, this procedure is typically completed in less than 90 minutes, compared to the five or six hours typically required in open approaches. The patient undergoes a twilight anesthetic state where they can respond but don’t remember anything.
“We can control the degree of sedation to allow patients to provide feedback on whether we have relieved the pain source,” Gardocki said.
Worth the Institutional Downside
Gardocki says this endoscopic transforaminal approach, although not entirely new, represents a dramatic shift from traditional methods and has been slow to take hold.
“It’s a lower cost to the patient, the insurance company, and society, but also lower revenue for both the hospital and surgeon,” Gardocki said. “Wherever this procedure is adopted, the center has to make a commitment to spend money on new equipment to make less, simply because it’s better for the patient.”
“Wherever this procedure is adopted, the center has to make a commitment to spend money on new equipment to make less, simply because it’s better for the patient.”
Gardocki is working with a handful of other surgeons performing this surgery through a multicenter collaborative team called the Endoscopic Spine Research Group, which is also evaluating outcomes.