Ovarian cancer is diagnosed in approximately 20,000 women annually in the United States. Efforts to screen by performing routine ultrasound and measuring serum CA 125, the most common ovarian cancer tumor marker, have proven ineffective in detecting these cancers at an early stage and reducing mortality. While these efforts are intended to identify and treat cases early, more than half of those diagnosed will still die from the disease.
Arthur C. Fleischer, M.D., the Cornelius Vanderbilt Professor of Radiology and Radiological Sciences and a professor of obstetrics and gynecology at Vanderbilt University Medical Center, has worked with ultrasound manufacturer Philips to develop software that enables clinicians to use 3D contrast-enhanced transvaginal ultrasound (TVS) for imaging microbubbles within the micro vessels of the fallopian tubes. This novel method could enable earlier diagnosis of high-grade serous cancer (HGSC) and its precursor lesions.
“We are targeting the more aggressive type II ovarian tumors that originate in the non-ciliated fimbriated end of the fallopian tube,” Fleischer explains. “Because ultrasound has come so far, we can now detect the increase in vascularity there that is a portent of ovarian tumor development.”
Fleischer and Ben Ho Park, M.D., Cornelius Abernathy Craig Professor of Medicine, are partnering with Vanderbilt colleagues Ronald Alvarez, M.D., chairman and clinical service chief of obstetrics and gynecology, and Marta Crispens, M.D., director of the Division of Gynecologic Oncology, to develop a pilot study of this approach. The study is funded by the Morrow family and Morrow Foundation.
Better Early Detection
HGSC, the most common and most lethal form of ovarian cancer, does not arise from the ovary but from the epithelium at the distal end of the fallopian tube. Moreover, its precancer lesions, serous tubal intraepithelial carcinomas (STICs), do not typically produce large masses that are easily detectable with conventional ultrasound. This understanding, and limitations of detection through CA 125, led to the search for a better way of detecting tiny HGSC and precancer STIC lesions.
“It’s really the first time, to my knowledge, that we’ve looked at the tube, as well as the ovary, as the origin of these aggressive tumors,” Fleischer said.
How the Screening Tool Works
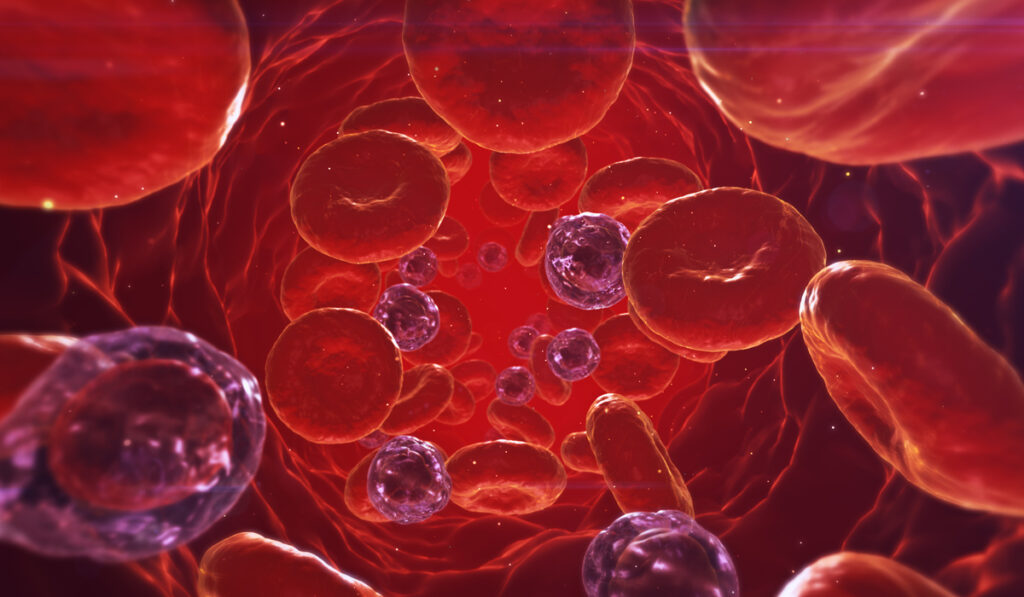
The new screening method involves injecting microbubbles directly into the venous system or through a uterine catheter, from which point they migrate to the fallopian tubes. The research team then employs a method for labeling these microbubbles with lipid shells for attachment to ligands that guide them to where abnormal vessels are developing.
The microbubbles are two-thirds the size of a red blood cell and oscillate at a harmonic frequency. This difference allows the investigators to use the harmonic mode of ultrasound to look at flow activity in tiny capillary-type vessels.
“It’s really the first time, to my knowledge, that we’ve looked at the tube, as well as the ovary, as the origin of these aggressive tumors.”
The imaging consists of a 10-second sweep of the area, producing a 3D volume from which images can then be sliced and diced to look for tumors in the distal portion of the tubes. Cancer is suspected when haphazard arrangements, vascular shunts, or longer blood-flow times are detected.
“This technique enables evaluation of the microvessels throughout the entire tube – which is a very tortuous structure – on a very minute scale,” Fleischer said.
Combination Approach
The researchers are combining the microbubble evaluation with cell-free DNA testing pioneered by Park. This technology constitutes a liquid biopsy to identify DNA in the bloodstream that may be associated with cancer. Circulating cell-free DNA can be analyzed for mutations and used to describe the tumor type.
The study focuses on patients with a BRCA mutation, which confers a lifetime risk of 44 percent (BRCA1) and 17 percent (BRCA2) for developing ovarian cancer. Such women often have their tubes and ovaries removed during their early 40s.
“This technique enables evaluation of the microvessels throughout the entire tube – which is a very tortuous structure – on a very minute scale.”
Study patients will undergo a 3D transvaginal microbubble ultrasound, as well as the liquid biopsy, prior to this surgery. Test results may then be correlated with any pathologic findings from serial section processing of the fallopian tubes and ovaries.
“Screening with TVS and CA 125 have not proven to be effective in decreasing mortality from this disease,” Alvarez said. “If we can prove that we can detect early-stage cancer or precancer lesions in women who have BRCA mutations, we can consider a study to evaluate these screening modalities in a larger population, both with and without a BRCA mutation.”