When diagnosing a patient who may be having functional seizures, the care team at the Vanderbilt University Medical Center nonepileptic seizure clinic proceeds systematically to evaluate the cause of seizures as psychogenic before instituting an underutilized but effective treatment.
“Nonepileptic seizure events really look like epileptic seizures,” said Andre Lagrange, M.D., an associate professor of neurology at Vanderbilt. “Neurologists watching videos of these seizures cannot always accurately tell them apart from epileptic seizures. For patients, they are scary as heck.”
Patients, as well as parents of affected children, often fear these seizures will cause death at night while the patient is sleeping and are frequently surprised to learn the seizures are a response to stress.
Detailed Diagnostic Process
The nonepileptic seizure clinic opened in 2021 and has helped about 45 patients during its first year, Lagrange said.
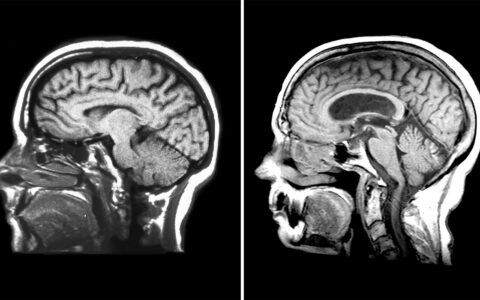
The epilepsy team verifies patients’ seizures are not physiologic by using electroencephalogram (EEG) testing, he said. They also take a detailed history to define how a typical seizure looks for that patient.
“For one patient, it may start with their left thumb twitching. With another, their head may start turning right,” Lagrange said.
The team videotapes the patient having a seizure in the epilepsy monitoring unit and shows the video to the patient’s relatives.
“We want to hear the relatives say, ‘That’s exactly what happens at home,’” he added.
Once a confident diagnosis of nonepileptic seizure is made, the patient may be referred to the specialty clinic.
“Neurologists watching videos of these seizures cannot always accurately tell them apart from epileptic seizures. For patients, they are scary as heck.”
When Stress Erupts
Within the field of psychology, functional seizures are called conversion disorders. The seizures are a visible manifestation – or “conversion” – of the person’s psychological distress, Lagrange explained.
“Everyone puts stress into their bodies in some way, though most of us don’t wind up having psychogenic seizures,” he said. “We may get migraines or backaches or grind our teeth.”
Once confirmed as seizures that are not epileptic, clinic experts assess the patient for a range of neurological conditions such as migraines, sleep disorders and movement disorders. If a problem is uncovered that is treatable with medications, a neurologist prescribes those medications. A team physician withdraws any unnecessary seizure medicines.
A psychiatrist will also assess each patient for other mental health conditions that may warrant treatment, such as anxiety or a mood disorder.
“Many people with functional seizures do not have other mental illnesses, but we screen for these things and treat them as necessary,” Lagrange said. “On average it takes five to 10 years to reach a diagnosis of functional seizures.”
Past Abuse Not Uncommon
Many with functional seizures report having sexual-, physical-, and/or emotional-abuse experiences in their history, Lagrange said. The psychiatry team routinely checks for post-traumatic stress disorder and other psychiatric comorbidities.
Routine mental health screenings have been put in place recently for patients with epilepsy, as well. Epileptic seizure patients report high rates of depression.
“We have an open invitation to therapists who want to learn to treat conversion disorders.”
Initiating Evidence-based Therapy
Patients with functional seizures typically receive referrals for talk therapy, but therapists are not always prepared to provide effective care in these cases.
“It’s like taking a 25-year-old to a pediatrician,” Lagrange said. “They might help with certain issues, but at some point the therapist will say, ‘I wasn’t trained for this.’”
In contrast, Vanderbilt’s clinic, housed within the Department of Neurology, employs a specific, effective form of cognitive behavioral therapy devised by W. Curt LaFrance Jr., M.D, a professor of psychiatry and neurology at Brown University. The program helps patients understand the emotional issues underlying their seizures and provides tools for managing stress and living a more fulfilling life, Lagrange explains. A workbook encapsulates the program.
“On average it takes five to 10 years to reach a diagnosis of functional seizures.”
A Unique Facility
Just a few other places provide this particular type of cognitive behavioral therapy, primarily within the Veterans Affairs system, Lagrange said. “But I don’t know of any facilities other than our own that have a collaborative team of neurologists, psychiatrists and psychologists each seeing a patient within a multidisciplinary clinic,” he said.
Because of this, Lagrange believes Vanderbilt’s program is unique, saying his team has fielded inquiries from clinicians elsewhere thinking about starting something similar.
“Providing training is a goal for us, and we have an open invitation to therapists who want to learn to treat conversion disorders,” Lagrange said.