No two glioblastomas are the same, but the most deadly have something in common: they recur after a period of time, says Lola Chambless, M.D., an associate professor of neurological surgery at Vanderbilt University Medical Center.
Chambless believes this characteristic may lead investigators toward identifying a common therapeutic target. “They’re exceptionally heterogenous,” Chambless said of glioblastomas. “There are a wide variety of characteristics that send them in totally different oncologic directions.”
“Current therapeutics target the majority of cells in a tumor, and they may be effective at preventing tumor growth, but if there is some small population that biologically escapes treatment, those are the cells we need to be exploring.”
Looking deeper, neurosurgeons at Vanderbilt are trying to determine whether certain stem cells may be responsible when tumors recur.
Precision Tissue Collection
Research into glioblastoma origin starts in the operating room. By performing subregion tissue collection, Chambless and her team of neurosurgeons are able to better characterize distinct cell populations within a single tumor. Coupled with cutting-edge technology such as exoscope-guided resections, neurosurgical approaches at Vanderbilt now allow precise sampling of different glioblastoma and brain cell populations with detailed spatial analyses.
“Tissue collection for glioblastoma in the past has primarily focused on analyzing the whole resected tumor. That can tell you common cell type proportions, but it tends to miss tiny subpopulations of origin cells,” Chambless said.
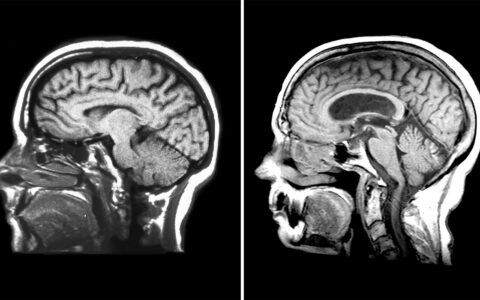
Through careful intraoperative sampling, the team is better able to elucidate cells in the subventricular zone, where glioblastomas often, but not always, arise.
Subventricular Findings
Chambless and colleagues already have discovered tumor contact with the subventricular zone is associated with decreased overall survival and early recurrence rates. Now, the researchers are isolating cells from this important region to understand why.
“Surgical debulking to decompress the mass effect and sample tissue is probably always going to be necessary, but ideally we are moving toward individualized, adjuvant therapy.”
Through single-cell analysis and other techniques, the researchers are able to study individual cellular features. These highly specific experiments are performed at Vanderbilt under the direction of long-time Chambless collaborators Rebecca Ihrie, Ph.D. and Jonathan Irish, Ph.D., both associate professors of cell and developmental biology.
“We’re comparing individual cells from the subventricular zone to those found in the rest of the tumor,” Chambless said. “In this way, we can not only learn mechanistic differences, but also begin to test therapeutics against origin cells in vitro.”
Toward Cell-specific Therapies
Their goal is to identify medical treatment that is specifically active against glioblastoma origin cells to prevent relapse and recurrence.
“Current therapeutics target the majority of cells in a tumor, and they may be effective at preventing tumor growth, but if there is some small population that biologically escapes treatment, those are the cells we need to be exploring,” said Ryan Merrell, M.D., division chief of neuro-oncology at Vanderbilt.
Identifying why some glioblastomas recur will likely not eliminate the need for surgery.
“Surgical debulking to decompress the mass effect and sample tissue is probably always going to be necessary, but ideally we are moving toward individualized, adjuvant therapy,” Chambless said.