A team of surgeons at Monroe Carell Jr. Children’s Hospital at Vanderbilt is the first in the country to use a new Connect EA magnamosis device to reconstruct the esophagus of a child suffering from a rare form of esophageal atresia.
Born with tracheoesophageal fistula Type B and tracheobronchomalacia, the infant’s underdeveloped esophagus collected secretions, causing recurrent pneumonia, while a collapsing airway hampered breathing. An international team of surgeons collaborated in a series of minimally invasive procedures to restore normal airflow and continuity of the esophagus.
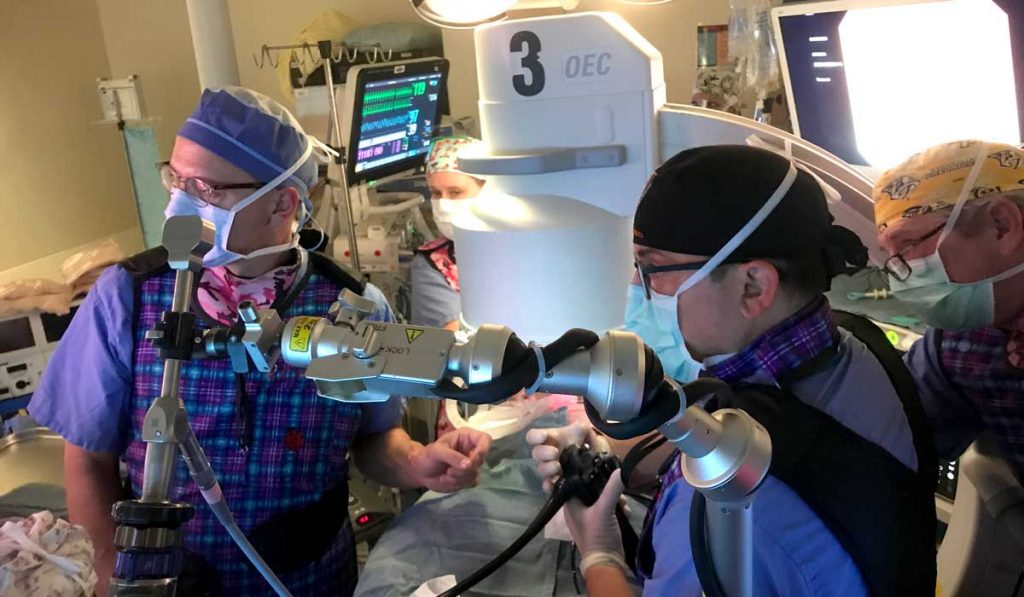
“This is a novel approach that essentially allows for endoscopic magnetic reconstruction of an esophagus and thoracoscopic opening of a collapsed airway,” said lead pediatric surgeon Irving J. Zamora, M.D. “Not many institutions are doing this, and even fewer are using a minimally invasive surgery approach to perform these innovative procedures.”
“This intercontinental, multi-institutional effort layered science, technology and the guidance of experts across the country.”
The Surgical Approach
The surgical plan required several steps. First, Children’s Hospital surgeons performed an anterior aortopexy and a thoracoscopic posterior tracheopexy to repair the 18-month-old’s damaged airway. Then, they performed the two-stage magnamosis procedure. The procedure was the first in the country to employ the new Connect EA magnamosis device created by colleagues at the University of California, San Francisco.
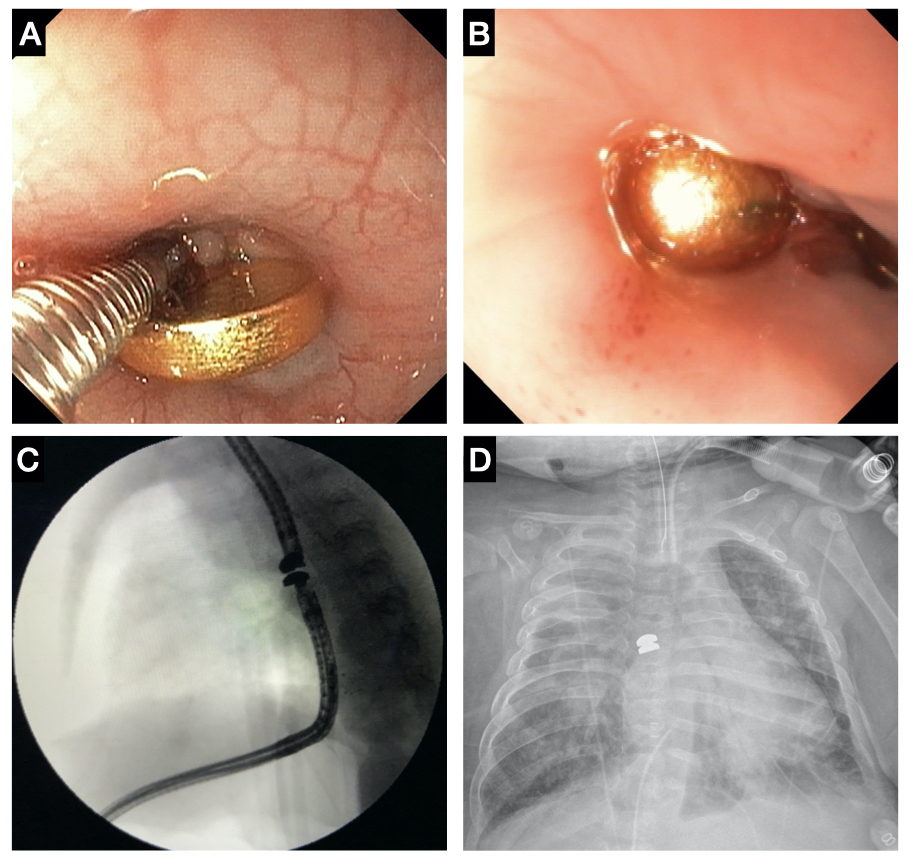
Magnamosis uses two ring-shaped magnets to connect parts to be anastomosed. It can be used to connect loops of intestine, or in the Children’s Hospital case, two ends of congenitally separated esophagus. The magnets, placed into each section of the tubular structures, bring them together while compressed tissue between the magnets necroses. Tissue forming around the magnets creates a patent lumen. The end result is a restored tubular structure.
At Children’s Hospital, the first stage of the innovative procedure involved suspending the upper part of the tracheal wall to the patient’s aorta. In a second operation several weeks later, Zamora and colleagues attached the lower portion of the airway to the spine, then anastomosed the two ends of the esophagus with the Connect EA magnets.
Said Zamora, “The use of the magnets was a minimally invasive way to create that connection without having to perform a complex and high-risk open surgery.”
Experts on Standby
Zamora, who is director of Advanced Minimally Invasive Surgery at Vanderbilt, said the Children’s Hospital team took months to prepare for the case, which required compassionate use approval from the FDA.
“This is a novel approach that essentially allows for endoscopic magnetic reconstruction of an esophagus and thoracoscopic opening of a collapsed airway.”
The collaborative endeavor also involved a live intraoperative Zoom conference with the device’s creator, Michael Harrison, M.D., as well as Oliver Muensterer, M.D. from Germany, who, to date, had been the only other surgeon in the world to ever use the device.
“This intercontinental, multi-institutional effort layered science, technology and the guidance of experts across the country,” Zamora said. “What would have been a potentially daylong, high-risk, open-chest and abdominal surgery was cut to a 38-minute endoscopic procedure.
Leap of Faith
Magnamosis is currently being tested as a minimally invasive approach for gastrojejunostomy, duodenostomy, and colocolostomy in adults. Magnamosis to repair congenital defects in an infant’s esophagus is a novel application performed at Vanderbilt.
Zamora says the young patient will remain tracheostomy and ventilator dependent in the short term but has stabilized and has been discharged home. The child is working with physical and occupational therapists to learn to swallow and no longer requires suction.
“This was a very, very sick baby when he first came to us, and over the course of the past year and a half we were able to rescue an incredibly complex patient and save his life,” Zamora said, adding, “Sometimes you have to take chances to make improvements, and you have to have someone willing to be the first.”