Researchers at Monroe Carell Jr. Children’s Hospital at Vanderbilt, Arkansas Children’s Hospital and Yale Craniofacial Center are using new imaging approaches to help clarify how craniosynostosis (CS) affects babies’ neurodevelopment. Diffusion tensor series imaging (DTI) and functional MRI (fMRI) will allow the researchers to observe, as never before, very small changes in brain structure and function before and after surgery.
Michael Golinko, M.D., chief of plastic surgery and director of the cleft and craniofacial program at Vanderbilt, and Christopher Bonfield, M.D., neurosurgery director of the Pediatric Craniofacial Program, are leading the study at Children’s Hospital.
“This study builds on Dr. Bonfield’s rabbit model and is the first study in humans with craniosynostosis looking at pre-surgery and post-surgery white matter tracts, correlating those data to neurodevelopmental testing, and comparing them to age-matched controls,” Golinko said.
“We hope these DTI studies will yield early biomarkers of brain abnormality.”
“One of the frustrations in explaining this surgery to parents is that we know shockingly little about what is going on in the child’s brain,” Golinko added. “We know that 10 to 15 percent of these children will develop high intracranial pressure, but by the time it is evidenced on a CT scan, the pressures have likely been longstanding. We hope these DTI studies will yield early biomarkers of brain abnormality.”
Providing Clinicians with Answers
The prevalence of elevated intracranial pressure in children with CS is as high as 20 percent in single suture synostosis and up to 60 percent in multi-suture synostosis. The resulting abnormal cerebral blood flow in areas of skull constriction contributes to potential white matter injury.
“We know that craniosynostosis affects each child differently,” Bonfield said. “The severity of the cosmetic appearance can vary significantly. Most patients undergo only one operation, but some require multiple surgeries and develop increased intracranial pressure.”
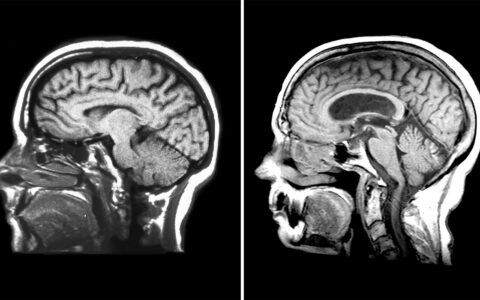
Bonfield says most babies with CS undergo either minimally-invasive endoscopic strip surgery between 10 weeks and 5 months of age or an open surgery between 6 and 12 months. Timing and procedure selection for each child are critical because their brains are rapidly growing, almost doubling in size over the first 12 months of life.
Study Design
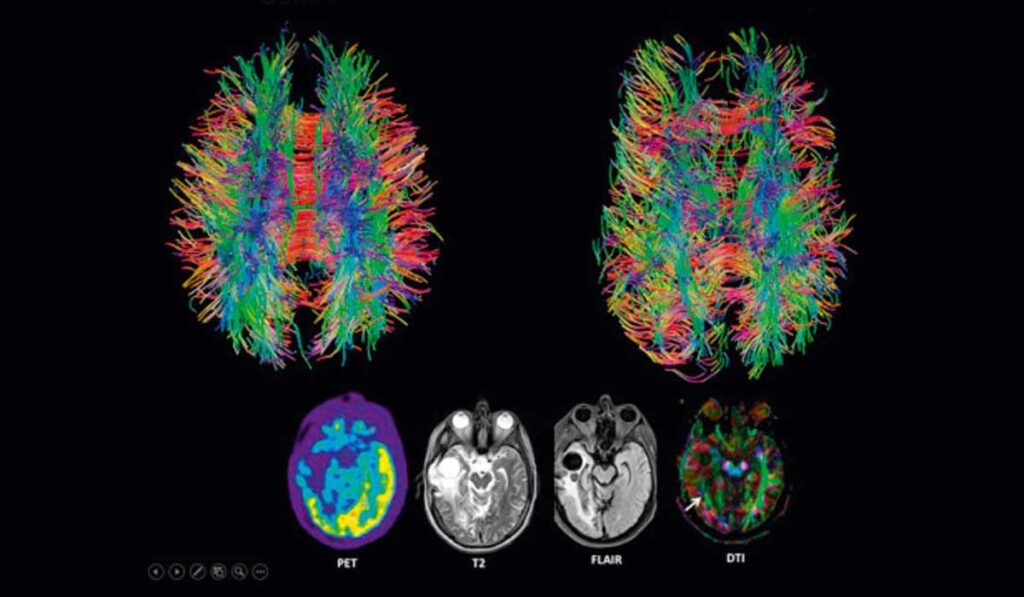
Diffusion tensor imaging works by delivering magnetic pulses in such a way that water molecules in the cell experience a random phase shift. This makes it possible to estimate the location, orientation, and anisotropy (the shift in water molecules) of the brain’s white matter tracts. Golinko has watched the evolution of DTI and envisioned its application to CS.
The researchers are pursuing three aims:
- Detect differences in fractional anisotropy in selected white matter regions of interest between children with and without CS;
- Quantify the impact surgery (either endoscopic or open) has on the white matter tracts in children with CS; and
- Measure differences in neurodevelopmental performance (using the Mullins scale) in children pre- and post-operatively.
Twenty babies with CS, at least 3 months old, will undergo MRI, fMRI, and DTI pre- and post-operatively. Using the Baby Connectome Project data, the researchers will compare their results with data from age-matched babies without CS. They hope to gather enough preliminary data to extend the study and obtain more imaging at a later time point. To date, the researchers have enrolled and acquired the scans and neurodevelopmental testing on four patients with different suture types of craniosynostosis.
Settling a Debate
Once they establish imaging biomarkers for white matter injury, the team plans to conduct a larger series exploring differences between minimally-invasive endoscopic versus open surgery, and what time point is ideal for surgery. While aesthetic outcomes may be similar for certain open and endoscopic repairs, Bonfield says there is still debate over which is better in terms of neuropsychological impact.
“We will have a more holistic definition of surgical success that encompasses not only aesthetics, but also the neuropsychological health of the baby.”
“If DTI proves to be a tool for detecting pressure increases earlier, we will have a more holistic definition of surgical success that encompasses not only aesthetics, but also the neuropsychological health of the baby,” he said.