Over the past 15 years, brain mapping researchers have discovered consistent evidence for the role of functional brain networks in controlling certain behaviors and symptoms, from delusions to criminal acts. Their research explains why people with lesions in different brain regions can share similar neuropsychiatric symptoms.
Ryan Darby, M.D., a neurologist and director of the Frontotemporal Dementia Clinic at Vanderbilt University Medical Center, recently earned the American Academy of Neurology 2020 Norman Geschwind prize for his work advancing research in functional brain networks. The prize recognizes the most outstanding research contribution to the field of behavioral neurology.
“Dr. Geschwind is considered to have founded the field of behavioral neurology in the modern era in the U.S.,” Darby said. “Our lab’s work has built on his network disconnection theory, validating that what once looked to be non-reproducible findings of discrete brain lesions are now explained by interruptions in the networks they share.”
“What once looked to be non-reproducible findings of discrete brain lesions are now explained by interruptions in the networks they share.”
This year’s award was based on Darby’s identification of functional networks associated with free will, criminal behavior and Capgras delusions (a belief that a family member has been replaced by an imposter). Currently, he is focusing on network connectivity in frontotemporal dementia.
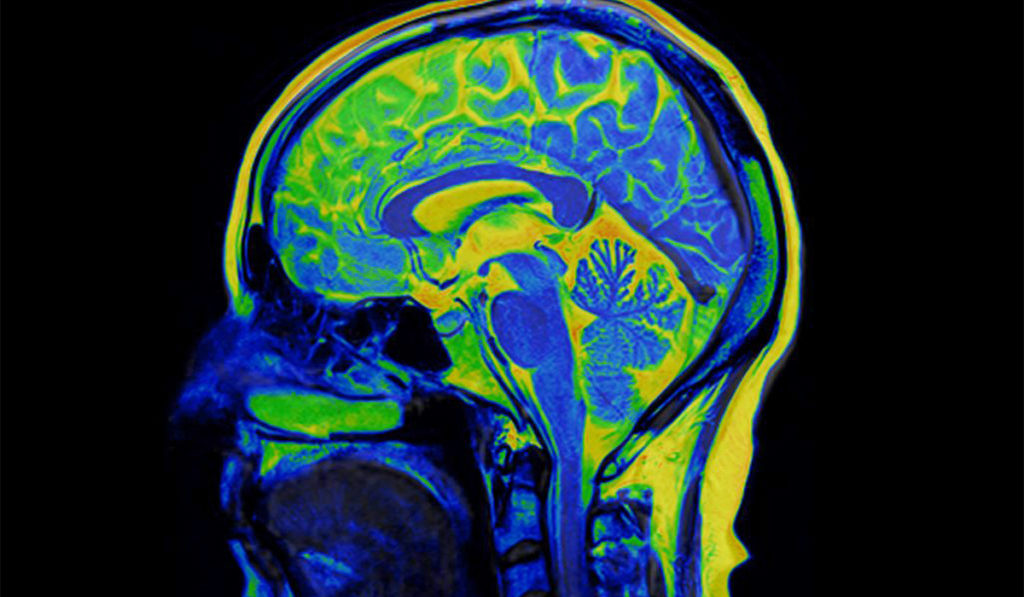
Visualizing the Network
Geschwind’s disconnection syndrome describes neurological symptoms caused by damage to white matter axons of communication pathways in the cerebrum, independent of any lesions to the cortex. Disconnection can occur anywhere in a given functional brain network and result in the same dysfunctional behavior.
A symptom such as criminal behavior may be due to a lesion in the frontal lobe, the temporal lobe, the amygdala, the nucleus accumbens, the ventral striatum or the basal ganglia area, Darby said.
Using fMRI, Darby and his team can visualize functional brain networks that span regions and hemispheres. When an individual’s brain damage is superimposed on the human connectome (a “wiring diagram” based on the average of over 1,000 brains), they can locate the sites of the lesions. Through watching areas where activity and dormancy are in synchrony, they can then identify the common networks.
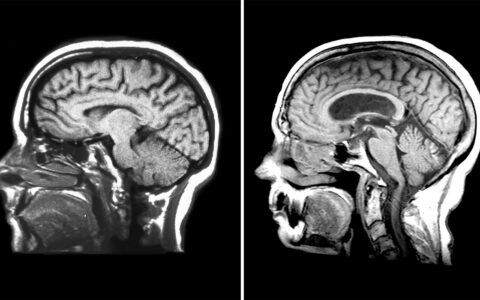
Cortical Atrophy and Dementia
“Frontotemporal dementia is the second most common form of dementia in people under 65,” Darby said. “Between 40 and 60 percent of [FTD] patients commit a crime, often non-violent, as part of their disease course. We’d like to understand if the same network is involved in different patients.”
“Between 40 and 60 percent of [FTD] patients commit a crime, often non-violent, as part of their disease course. We’d like to understand if the same network is involved in different patients.”
Darby and his team are using the human connectome to look at networks associated with cortical atrophy in dementias. Mapping these networks is particularly nuanced, Darby said. Unlike visualizing lesions, discerning and measuring a thinning cortex is difficult to do with the naked eye. “Fortunately, we can use computer algorithms as better ‘eyes’ for comparing these brains to normal brains,” he said.
Darby was the primary investigator on a recent study that looked at delusions, memory deficits and other syndromes found in Alzheimer’s disease. The researchers found that a thinning cortex along one of several points in a network accounts for common symptoms of delusion or memory deficits.
”Despite the heterogeneity of atrophied regions at the single-subject level, we found that 100 percent of patients with a clinical diagnosis of Alzheimer’s disease had atrophy functionally connected to the same brain regions in the mesial temporal lobe, precuneus cortex, and angular gyrus,” the authors wrote.
Research with Broad Implications
Building a library of these functional networks – and the pathologies and behaviors that reside in each – promises to elucidate a variety of pathologies.
“This work has important implications for psychiatry and public policy,” Darby said. “Most criminal acts are not committed by people with brain lesions or atrophy, but when we understand the anatomical basis for those that are, it changes the lens on how we view crime and punishment.”