Researchers are embarking on a prospective trial of the BlueWind Renova iStim™, a small, implantable tibial stimulation system for telemedicine-based treatment of overactive bladder (OAB). In Neurourology and Urodynamics, a recent pilot study of 20 patients with OAB demonstrated high three-year efficacy using the system, with 75 percent of patients gaining improved control.
“This technology offers completely at-home treatment, like a pacemaker does.”
Roger Dmochowski, M.D., associate surgeon in chief at Vanderbilt University Medical Center, served as medical monitor for the pilot study. “This technology offers completely at-home treatment, like a pacemaker does. It sends patient response data to physicians remotely, so they can then make satellite-based changes. It also allows the patient to regulate the stimulation themselves,” he says.
While neuromodulation is still considered secondary to medication, these outcomes may prompt patients to self-select it as first-line therapy when they are contraindicated for OAB drugs, or are simply seeking a non-systemic alternative. “Renova is a very unobtrusive device, implanted in an ambulatory environment, under local anesthesia, obviating the need for a directed implant with its much higher expense threshold,” Dmochowski says.
Options in Pelvic Neuromodulation
Up to 40 percent of women (mostly post-menopausal) have OAB, with symptoms ranging from urgency to leakage to incontinence. Over the past two decades, neuromodulation alternatives have been available to patients who fail, are contraindicated or who discontinue medication therapy.
The Renova is a pacemaker-sized device surgically implanted under anesthesia into the sacral complex, with stimulation controlled externally. While long-term follow-up studies are still ongoing, six-month and three-year clinical success rates for this procedure have been high. However, efficacy must be weighed against the cost and complications associated with surgery and abdominal implants.
Alternatively, patients can have percutaneous tibial nerve stimulation therapy in the outpatient clinic setting, through weekly 30-minute sessions. This involves electrical stimulation by cephalad insertion near the medial malleolus, with a surface electrode on the arch of the foot delivering the current. These sessions typically span 12 weeks, followed by periodic treatment as needed. While enjoying success, this method is time- and resource-intensive.
Acupuncture Roots
“There’s historical evidence that it works.”
The target for Renova implants and percutaneous tibial nerve stimulation devices is an acupuncture point that has been used by the Chinese for millennia. “Obviously, there’s historical evidence that it works,” Dmochowski said. “This particular application and approach was extrapolated by a very smart inventor about 30 years ago to create the first iteration of this technology. Now, we’re in the third or fourth generation of that technology.”
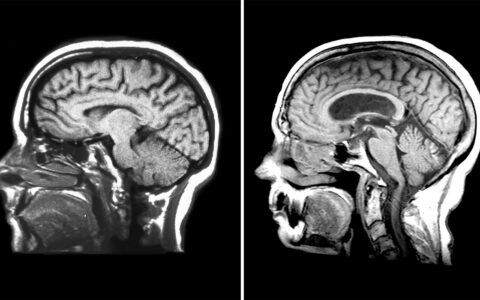
Stimulating the tibial nerve sends electrical current up the leg and into the sacral complex. Since the urinary process is complex, involving some volitional control, proper function requires an intact nervous system in the pelvic region, in the bladder specifically, and in the brain. Therefore, stimulation is designed to extend both to the regional nerves and up through the central nervous system to the brain.
Renova Benefits
With the Renova option, a surgeon implants a thin 3cm titanium rod at the ankle, near the tibial nerve. Stimulation occurs by activating an external control device (which has multiple settings) to send current from a small power stimulator worn around the ankle, that has radio frequency communication capabilities. Patients can track voiding patterns or simply self-report their level of symptom relief to the physician, triggering telemedicine adjustments in stimulation strength and session frequency.
For this pilot, patients completed a treatment cycle at home for 30 minutes daily. Historically, the percutaneous technique has been used anywhere from 6 to 12 weeks, followed by once a month ad infinitum, Dmochowski says. “The Renova technique, however, will be customized to each patient, with stimulation being adaptable to patient needs and lifestyle.”
“The big benefit of the device is that the individual can make it work with their daily activities,” he says. Further, he notes that emerging concerns about the association between some OAB medications and dementia may make neuromodulation a more attractive alternative to the millions of OAB sufferers.