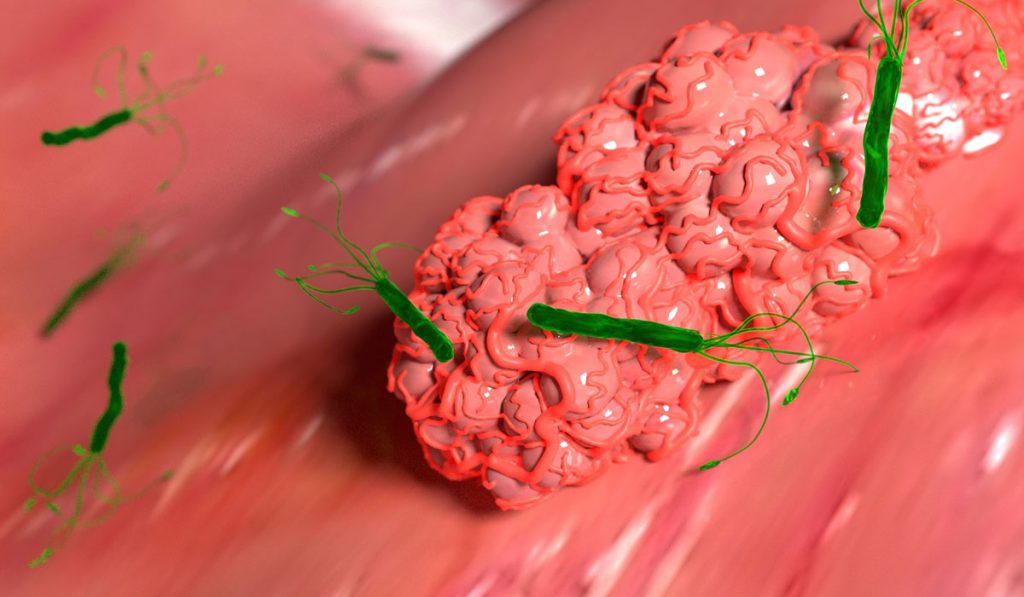
Gastric cancer, the third leading cause of cancer-related deaths worldwide, develops as a result of parietal cell loss, spasmolytic polypeptide-expressing metaplasia (SPEM), and intestinal metaplasia (IM), all considered precancerous lesions. Studies have shown that chronic inflammation resulting from Helicobacter pylori, a common bacterial infection, can induce metaplasia in the stomach.
Earlier this year, Cancer Research UK awarded a $26 million grant focused on inflammation-related cancers to an international team including James Goldenring, M.D., Paul W. Sanger Professor of Experimental Surgery at Vanderbilt University Medical Center. Goldenring, a site PI in the study, will focus on gastric cancer. Goldenring will investigate the impact of stroma – the connective cells in the stomach – and how it influences inflammatory responses and disease progression from pre-cancerous lesions to cancer.
“Almost all GI cancers are related to or are associated with inflammation,” said Goldenring. “With this grant, we will look at the interactions between the cells lining the stomach, colon and esophagus with their underlying stroma cells.”
Pre-Cancerous Organoid Models
Goldenring’s lab developed the first pre-cancerous organoid stomach models and will be using the same technology in the Cancer Research UK grant. The model is an in vitro system in which stomach cells are grown as 3D metaplasia comprised of spheres of cells or more complicated structures. The goal is to recreate renewable resources that anyone can use for research and testing drug therapies.
“The metaplastic organoids are much better than just working with a cancer cell line,” Goldenring said. “These ‘mini-stomachs’ can recapitulate many of the characteristics of the real lesions in the animal or human. We can combine them with elements of the immune system or the stroma to identify the interactions that may drive or regress pre-cancerous lesions.”
Reversing the Metaplastic Process
The organoid studies will build on Goldenring’s previous mouse work. In a study published in Gastroenterology, Goldenring and Eunyoung Choi, Ph.D., assistant professor of surgery, discovered that activation of signaling pathways by the protein K-ras (a strong oncogene that is mutated in many cancers) leads to the progression metaplasia and progression to intraepithelial neoplasia.
K-ras mice developed metaplastic glands, which led to the full range of metaplastic lineage transitions, including SPEM and IM. Selumetinib, a MEK (MAPK ERK kinase) inhibitor, induced regression of SPEM and IM, and re-established normal mucosal cells. The study results suggested the possibility of using selumetinib to prevent gastric cancer in patients with metaplasia in the stomach.
In a more recent Gastroenterology study, Goldenring and colleagues were able to interrupt and reverse the entire metaplasia process with the MEK inhibitor and allow re-emergence of normal lineages in gerbils who had been infected for one year with Helicobacter pylori. The researchers can now use their organoid system to further test these interventions, providing a firm foundation for clinical trials.
Benefits for Patients
“The good news is that we can ‘turn back’ metaplasia if we use these drugs.”
“The good news is that we can ‘turn back’ metaplasia if we use these drugs,” Goldenring said, “but getting approval to test them in humans is difficult. They have been used in stages III and IV cancers and have high side-effect profiles. The amounts we want to use are six to ten times lower.”
The patients Goldenring hopes to treat are those with stage I cancer resected by endoscopy, who have a 2-3 percent chance per year of developing a new cancer: “It’s a lot more cost effective to deal with early lesions; when you’re treating an early cancer, you want to have a drug with essentially no side effects.”
Choi is the Vanderbilt site co-investigator on the Cancer Research UK-funded project. Jimin Min, Ph.D., a postdoctoral fellow, will assist Goldenring and Choi.