“A third of the patients who come to us with STS have undergone an incomplete excision, requiring re-excision.”
Soft tissue sarcomas (STS) are rare tumors occurring in as few as 6 in 100,000 people, often assumed to be lipomas. The misdiagnosis and treatment of STS puts patients at risk for unnecessary morbidity and poor prognoses. Studies show that up to half of patients with STS undergo a first surgery designed to remove a benign tumor, not cancer.
“A third of the patients who come to us with STS have undergone an incomplete excision, requiring re-excision,” said Ginger Holt, M.D., an orthopaedic surgeon and sarcoma specialist with Vanderbilt University Medical Center. “Most of these patients have been through what we call a ‘whoops’ procedure: the surgeon thought they would be operating on a lipoma and then were caught off guard in finding something that is obviously not a fatty mass.”
The results are often severe, Holt said. “These patients can face massive re-excisions, putting them at greater risk for infection, pain, disfigurement, skin stiffness, additional radiation and higher odds of local recurrence.”
Identifying Barriers to Optimal Care
Holt led a team at Vanderbilt investigating where the gap lies between a patient presenting with an STS and a planned oncologic surgery. “How do the patient, the physician and the interaction between them, within the medical system, create this problem? And how can we eliminate it?” Holt asked.
They studied survey data on a number of potential influences on the “whoops” factor, including distance from a qualified treating facility, misunderstandings about the consequences of an incomplete excision, and patient requests that the biopsy and excision be done in the same setting. They also probed the impact of pay and other incentives to excise, and whether the low incidence of STS dissuades physicians from referring patients for imaging and pathology.
“While some of these factors likely play a role, none appeared to be a primary reason why ‘whoops’ procedures are so prevalent,” Holt said.
A nationwide survey assessing the knowledge and education of general and orthopaedic surgery residents led to a more concrete explanation. Holt’s team found that until 15 years ago, sarcomas were scarcely mentioned in general surgeons’ training and board preparation materials, leaving a gap in practicing surgeons’ skill set. Often, internist training does not cover STS at all. The relative rarity of soft tissue sarcomas (versus lipomas) compounds this training deficit. Most PCPs, general surgeons and some orthopaedic surgeons may never have seen one in a clinical setting.
A Prescription for Scrutinizing Lumps, Bumps and Masses
Holt is campaigning to address this educational gap, beginning at home. To ensure residents at Vanderbilt understand how to recognize potential STS, Holt created online educational modules that have been incorporated into surgical education programs. She has led an American College of Surgeons symposium on STS for the past six years, “to make sure we educate general surgeons as well as orthopaedic surgeons,” Holt said.
Holt’s training includes the simple protocol for evaluation shown here.
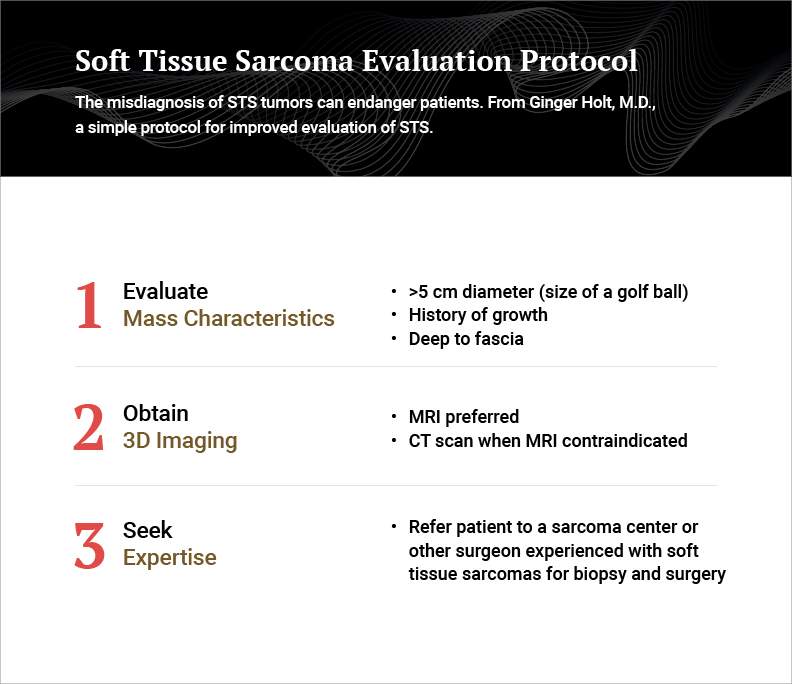
Physicians’ practices are rarely far away from a sarcoma center. Holt suggests the American College of Surgeons or Musculoskeletal Tumor Society websites for an easy referral process.
”The biggest improvement will come with primary care physicians being aware of these rare tumors and asking themselves, ‘Is it big, is it painful and is it growing?’” Holt said.
True Costs of Misdiagnosis
Insurance companies and government payers also need to dissuade surgeons from operating on lumps, bumps or masses until they have done a basic evaluation, and to reimburse for the right costs. While insurers may balk at the expense of a biopsy and re-imaging at a referral center, this is dwarfed by the cost of re-excision.
”Add to that the cost of treating post-operative morbidity, plus quality of life issues, and the case for treating every lipoma as a potential sarcoma is strong,” Holt said.