When a child has recurrent croup that hasn’t responded to multiple courses of steroids or when an adult has wheezing, coughing or shortness of breath, the problem may be an abnormality in the airway. Several complex diseases can cause this abnormality, but the diagnosis could be laryngotracheal stenosis, a rare condition in which part of the airway (larynx, trachea, carina or main bronchi) has narrowed or become misshapen and distorted.
In pediatric patients, laryngotracheal stenosis is usually subglottic and can result from a congenital condition such as laryngeal cleft, infection or trauma at birth, or long periods of intubation, especially in premature infants. Adults are at risk for laryngotracheal stenosis who have had prolonged intubation following pneumonia, a heart attack or surgery or trauma in the neck or chest. Middle-aged women of Northern European descent develop idiopathic laryngotracheal stenosis, possibly relating to an infection or an immunologic disorder.
“These are complex patients with unique inflammatory conditions. As a surgeon, you want to find the best anatomical solution.”
Esophageal problems and other digestive conditions can also affect tracheal tissue and impact airway function. “These are complex patients with unique inflammatory conditions,” said Christopher Wootten, M.D., Director of Pediatric Otolaryngology at Vanderbilt University Medical Center. “As a surgeon, you want to find the best anatomical solution. We get optimal outcomes when diagnosis takes a multidisciplinary approach. That includes a team of otolaryngologists, pulmonologists, gastroenterologists and radiologists.”
Diagnosis and Treatment
The most reliable and most commonly utilized approach for diagnosing complex airway disease is endoscopy. CT and MRI scans can be useful in further defining the problem, and laryngoscopy, bronchoscopy or esophagoscopy may be used to confirm the diagnosis and determine treatment. “It’s important to conduct a full battery of labs to understand the cause of inflammation and the structural issues at play,” said Wootten.
Treatment of laryngotracheal stenosis depends on the location and severity of the stenosis. Dilation — either with a balloon or tracheal dilators — can widen the trachea and provide temporary symptom relief. A stent may be placed at the site of the stenosis to help keep the airway open. Laser surgery can provide short-term relief but usually isn’t a lasting solution and, in some cases, can make the stenosis worse.
A more complex approach is cricotracheal resection, for patients who have a short section of scarring at the level of the cricoid and the tracheal segment immediately below it. The surgery removes the scarred portion of the airway and reconnects the healthy ends. In highly experienced centers, laryngotracheal resection and reconstruction with a graft from ribs or other tissue is currently the best alternative to completely cure the stenosis.
“The goal,” explained Wootten, “is to support the framework and get the epithelial tissues working again to remove bacteria and other particles out of the lungs to allow for the circulation of mucus and saliva.”
Latest Innovations
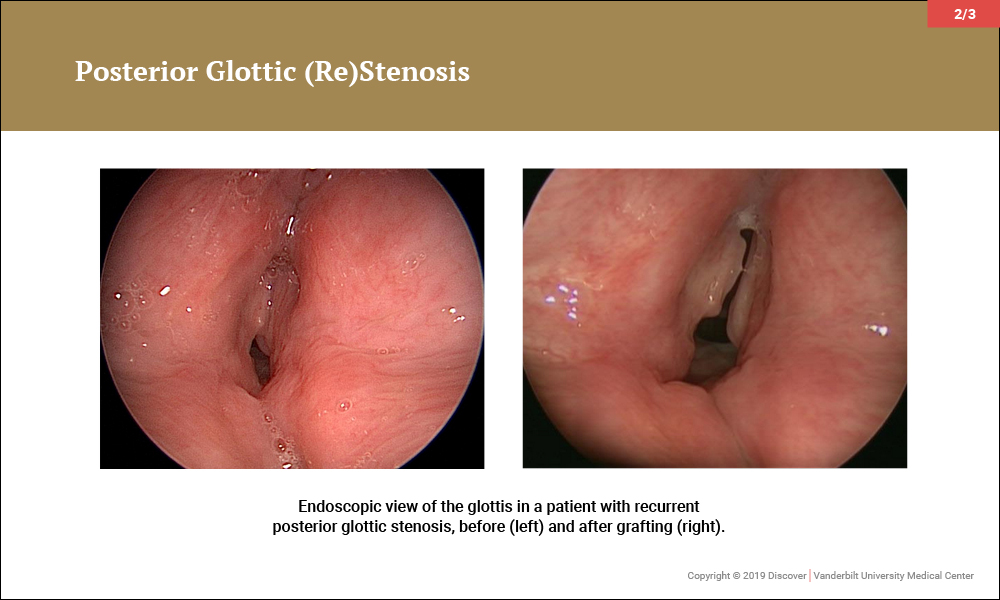
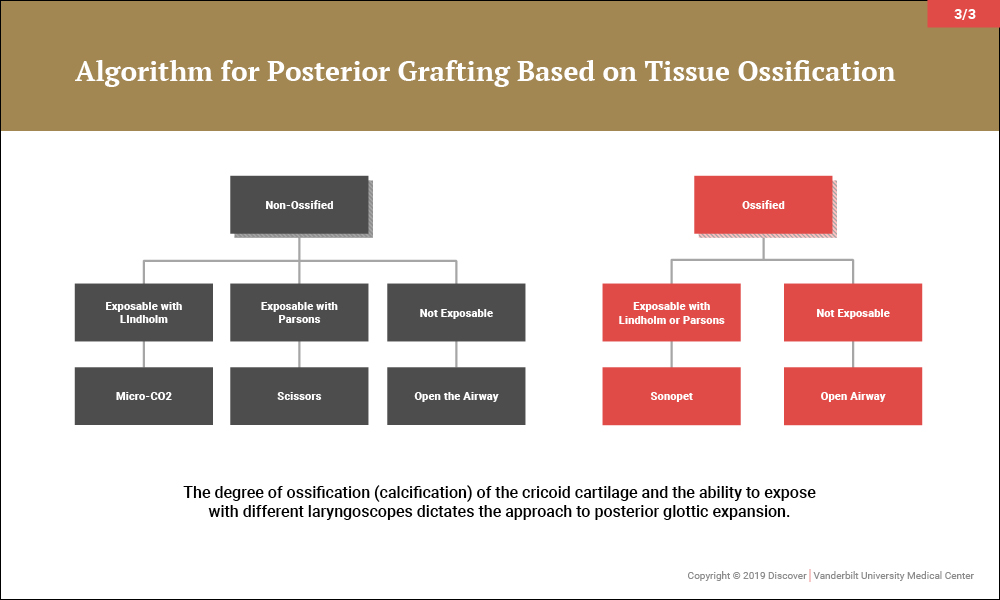
In the last several years, investigators at Vanderbilt have refined the technique (described originally by Inglis) for endoscopic expansion of the posterior glottis. In adults with highly calcified cricoid cartilage, an ultrasonic aspirator is used to split the larynx. In non-calcified adults and children, an algorithm has been developed that uses endoscopic scissors to split the cartilage, emphasizing submucosal division of the posterior plate of the cricoid and graft placement whenever possible.
“These techniques offer certain patients relief of posterior glottic stenosis resulting from scar,” said Wootten, “with less joint immobility, paralysis, or morbidity than with traditional ‘open’ approaches.”