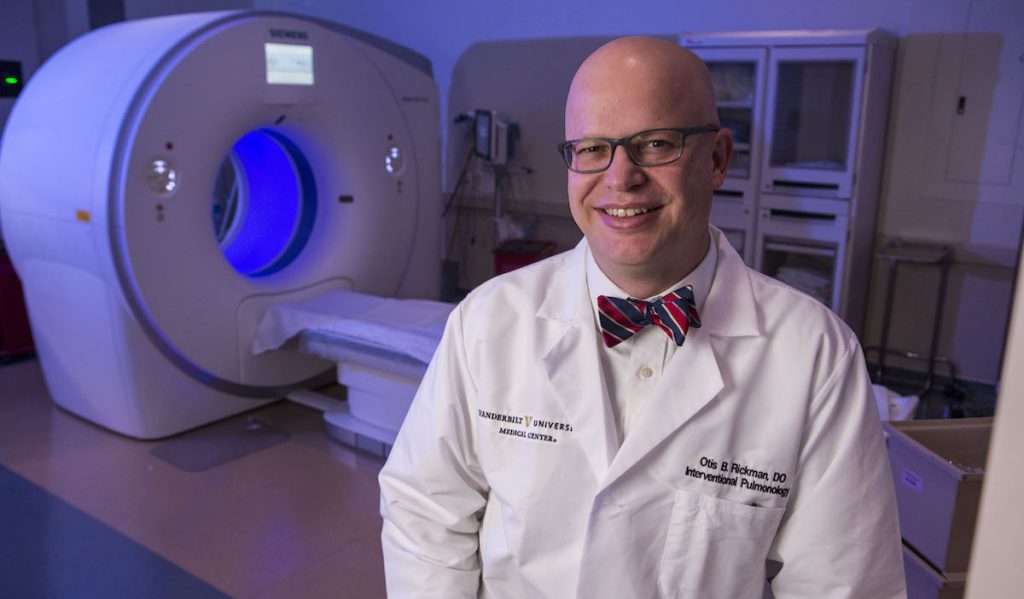
Otis Rickman, D.O., joined Vanderbilt University Medical Center the same year he founded its Interventional Pulmonology Program, in 2009. Below, a conversation with Rickman about the past and future of the program and how technology is advancing the field.
Discoveries: You’re the founding director of the Interventional Pulmonology Program, which began at Vanderbilt back in 2009. Describe the growth of the program.
Rickman: I was recruited from Mayo Clinic to Vanderbilt to start the Interventional Pulmonology Program. Up to that point, we had a typical university-based pulmonology program doing about 500 bronchoscopies or so a year. Most of those were inpatients. We had no advanced diagnostic or therapeutic capabilities, so there was a big push from the university to provide that service to the people in Middle Tennessee, and especially here in the Nashville area.
“We have gone from doing about 500 bronchoscopies or interventional procedures a year to over 1,500. The program has tripled in size… we’ve been able to bring minimally invasive diagnostic and therapeutic procedures that were otherwise unavailable to people across the state.”
There was a lot of support from the university — capital outlay, funds, equipment and personnel — to make this the first interventional pulmonology program in Tennessee. To this day, it remains the only true interventional pulmonology program in Middle Tennessee with board-certified interventional pulmonologists. Over the past seven or eight years, we have gone from doing about 500 bronchoscopies or interventional procedures a year to over 1,500. The program has tripled in size in that time period, and we’ve been able to bring minimally invasive diagnostic and therapeutic procedures that were otherwise unavailable to people across the state.
Discoveries: In terms of patient care, what has developing this expertise allowed you to provide in addition to what was already available?
Rickman: Interventional pulmonology as a subspecialty relies on minimally invasive bronchoscopy and pleural procedures to reduce patient discomfort or risk for procedures that would have normally been a hospital stay or a high-complication rate. This includes navigational bronchoscopy, which is when a computer takes a radiology scan from a CT and molds them both together. We’ve been doing that procedure to do lung biopsies of nodules. That wasn’t being done in Tennessee.
We also started doing a procedure called endobronchial ultrasound, which uses a small, flexible scope within the bronchoscope along with ultrasound. We can see through the wall of the bronchial tubes and identify lymph nodes, then put a needle into those and do staging that previously would require a big cut right above the breastbone and a stay in the hospital. We’re able to provide that as an outpatient procedure.
Those two have been the most used of our advanced diagnostic bronchoscopy procedures. Then, a couple of years ago, we added Fabien Maldonado, M.D., another board-certified interventional pulmonologist. Maldonado brought expertise in medical pleuroscopy, which utilizes a miniature scope, slightly different, to go in between the ribs while the patient is spontaneously breathing. With just local anesthetic, we can look at the space around the lungs for any diseases in the chest, take biopsies and actually perform interventions. Patients go home the same day.
Discoveries: How do you connect with patients who might benefit from these procedures?
Rickman: We’re lucky to be at a place like Vanderbilt, with Vanderbilt-Ingram Cancer Center being the only adult NCI-recognized comprehensive cancer center in Tennessee. Because of that, we get patients who are referred in for lung cancer and need additional testing, or additional procedures for therapeutic reasons. Patients also self-refer in. Usually that is from the Nashville area, but we also see patients from across Tennessee, Alabama and Kentucky.
For some of our research trials in interventional pulmonology, people may come from several states away or nationally. A lot of times, patients who are referred in from the farthest distance have obstructed airways from cancer. We do a procedure called rigid bronchoscopy that relieves the obstruction causing shortness of breath or coughing up blood, then we place stents and use laser therapy to remove the cancer in the bronchial tube. It really improves patients’ quality of life.
Discoveries: Lung cancer screening is one of our strengths. What exciting work are we doing in cancer screening?
Rickman: We’ve been doing research with Pierre Massion, M.D., for many years looking at different methods for lung cancer screening. In January of 2016, the Centers for Medicare and Medicaid Services approved national lung cancer screening as a covered benefit for people with Medicare, so that has supported us in setting up an extensive screening program for patients across the region. That program will really change how we’re diagnosing lung cancer.
Lung cancer is the No. 1 cancer killer in the United States. It has no symptoms and presents late when it’s not curable. Through our screening program, we can detect these cancers with a CT scan before they become invasive or non-curable with surgery. We’ve established this program in collaboration with our radiology department; we have a nurse practitioner and the infrastructure to automate follow-ups, return scans and paperwork. It’s easy for patients to get in and out, very similar to how women get mammograms.
Discoveries: Where does the Interventional Pulmonology Program stand today in terms of the size of the program, resources and your progress toward your goals?
Rickman: When we started, we were trying to establish a program that would benefit patients in Middle Tennessee. Next, we wanted was to become a nationally prominent program. Both Dr. Maldonado and I are board certified and sit on the board of directors of the American Association of Bronchology and Interventional Pulmonology, the national certifying organization for interventional pulmonologists. We have also been instrumental in establishing training program guidelines for interventional pulmonologists. We both sat on the committee that developed guidelines for all training programs in the United States.
Discoveries: Advanced technology is so important to your field. What are we exploring in terms of new technologies?
We have several external grants for independent research. In conjunction with the Vanderbilt Department of Engineering, we have two grants looking at robotic-assisted bronchoscopy, including a steerable robot needle that will even more efficiently biopsy lung nodules. My ultimate desire would be to not only biopsy the lung nodules, but after we identify them to ablate them. By ablate, I mean cryotherapy or some sort of ablative therapy. The first we’ll use may be microwave.
“My ultimate desire would be to not only biopsy the lung nodules, but after we identify them to ablate them. By ablate, I mean cryotherapy or some sort of ablative therapy. The first we’ll use may be microwave.”
We have also received an R01 grant for an endoscopic robot that we’re able to introduce down past the vocal cords and into the windpipe. It significantly improves our ability to interact with tumors in the airways, and it allows us to resect tumors with finer control than what we had in the past.
We’ve worked very closely with a lot of tech industries, especially medical devices, to get the latest technology at Vanderbilt and serve as consultants and advisors to those companies. Because of that, we have several ongoing clinical trials looking at exciting things like using a valve to treat emphysema patients. That is placed, again, via bronchoscope, so it’s a procedural treatment for emphysema that we hope will improve dyspnea or shortness of breath and improve quality of life. We also participated in usability studies for another device for emphysema, which was a nitinol coil that clamps down and causes lung volume reduction. Last year, we completed a large trial looking at navigational bronchoscopy that we hope will give us a real-world use summary of how effective navigational bronchoscopy is for identifying lung nodules, among a few things.
Discoveries: If a patient or a patient’s physician feels that they may benefit from one of these trials, what’s the best way to learn more?
Rickman: Information on individual trials is available on our clinical trials website. There’s also an interventional pulmonology page within the Department of Pulmonary Medicine website. We are happy to receive any patient referrals by phone at (615) 936-8422.
Discoveries: Looking forward, what most excites you about the field of interventional pulmonology?
Rickman: Especially for lung nodules, I think we’re going to be moving away from just diagnosing to treating. Dr. Massion has been working on blood tests to detect lung cancer, so we won’t have to go in and do biopsies anymore. We’re going to be treating lung cancer more minimally invasive, instead of having to do a big incision and removing it. That’s going to include robotic bronchoscopy and ablation of those lung nodules.
I’m most excited that we’ve positioned ourselves at Vanderbilt with the infrastructure and capital to offer those services when the technologies become available, either in clinical trial or immediately after the clinical trials.
Discoveries: Thank you for talking with us about the beginnings of this unique program and where the field is headed. It’s very exciting.
Rickman: Thank you.