Currently, ongoing evaluation of children’s eosinophilic gastrointestinal disorders (EGIDs) requires repeated endoscopies and biopsies. This is time consuming, expensive and stressful for the patient, but it is necessary to identify and treat EGIDs before they cause potentially irreversible tissue damage and fibrosis.
The most common EGID, eosinophilic esophagitis (EoE), is being increasingly recognized among children and adults. “It appears to be a manifestation of an allergy to foods, or less commonly, to aero-allergens,” said Sari Acra, M.D., division chief of Pediatric Gastroenterology, Hepatology and Nutrition at Monroe Carell Jr. Children’s Hospital at Vanderbilt.
At Vanderbilt, pediatric gastroenterologists are working to improve the evaluation of EoE and other EGIDs after initial diagnosis through a robust clinical and research program led by Girish Hiremath, M.D. The team’s current focus is on advances that could help children and their families avoid the stress of repeated endoscopies and biopsies.
Toxic Consequences
In EoE, an allergy-triggering substance enters the esophagus prompting an excessive quantity of eosinophils to migrate to the affected area, releasing large quantities of toxins.
Explained Hiremath, “These toxins can lead to uncontrolled and chronic inflammation which, in turn, can lead to irreversible tissue damage and long-term consequences such as dysphagia and esophageal remodeling.”
Such complications may require repeated invasive procedure including esophageal dilations, highlighting the importance of accurate diagnoses.
“It can be difficult to distinguish EoE from other conditions that affect the esophagus. One such common disorder is gastroesophageal reflux disease or GERD,” Hiremath said. “More convenient and accurate diagnostic tools could lead to early identification of EoE, which could potentially prevent the occurrence of irreversible tissue damage.”
“Our research is not just about diagnosing the disease – it’s also about figuring out what resources the families need to overcome it.”
Novel Technologies Ease Procedures
One promising diagnostic tool under investigation is a novel, non-invasive fiber-optic Raman spectroscopy probe. Hiremath and colleagues are testing if the probe could identify unique biochemical signatures for EoE, GERD and other overlapping conditions in real-time to enable more accurate differential diagnoses.
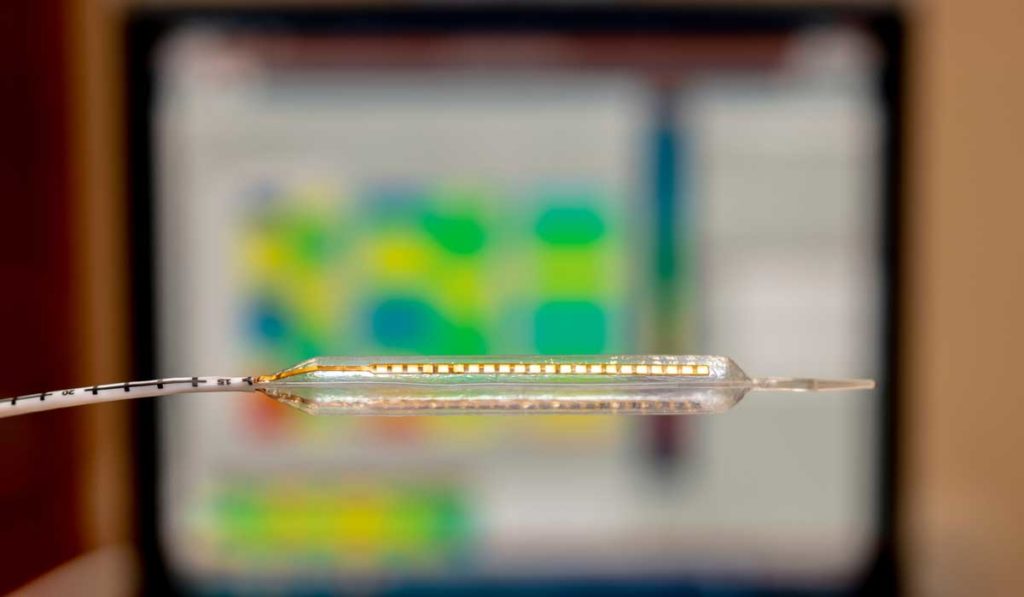
Acra is also repurposing probe technology developed at Vanderbilt for adult GI patients to detect electrical resistance in the esophagus. By touching the surface of the esophagus, the technology measures mucosal impedance to reveal the level of tissue inflammation.
Finally, the researchers are exploring the prospect that changes in the salivary microbiome play a role in EoE pathobiology and could be a marker of the disease. Work by Hiremath, Acra and others found pediatric patients with EoE have more Haemophilus species in their saliva, along with lower microbial richness and diversity.
Hiremath says these new diagnostic technologies will contribute new understanding of the pathophysiology of EGIDs. Raman spectroscopy, for example, could lead to insights into biochemical changes that drive disease evolution from an inflammatory to a fibrostenotic phenotype.
Improving Care for Patients and Families
Acra adds that along with introducing tools to make procedures more comfortable, the Vanderbilt program remains focused on the broad picture for patients and their families. “Our research is not just about diagnosing the disease – it’s also about figuring out what resources the families need to overcome it.”
The team recently shed light on the difficult experiences of patients with EGIDs and their caregivers in a survey-based study. “This study is an important first step in addressing the gap in medical and emotional support for patients and caregivers of those affected by EGIDs,” Hiremath said.