Cardiomyopathy is the leading cause of death in Duchenne muscular dystrophy (DMD), the most common form of muscular dystrophy. Yet there are broad variances in age of cardiomyopathy onset, and currently there are no effective genetic, blood or imaging biomarkers for predicting the timing. There are also no DMD-specific cardiovascular therapies.
The FDA recently awarded a $2.4 million rare disease grant to Jonathan Soslow, M.D., co-director of the Duchenne Muscular Dystrophy Clinic at Monroe Carell Jr. Children’s Hospital, to identify DMD biomarkers. This prospective research falls under a larger umbrella of mapping the natural history of the disease.
“One of the outcomes we hope for is a blood or imaging test that can better tell us how we can expect cardiomyopathy to progress in boys with DMD,” Soslow said.
The Search for Biomarkers
There is significant variability in the cardiovascular progression of DMD. One young man may have normal left ventricular ejection fraction in his twenties, while another will have significant cardiomyopathy before he is a teenager. Soslow says knowing who is destined for which path is the first step in personalized treatment. “Looking for these biomarkers, whether or not disease-specific, may help us find novel pathways that lead to therapeutic interventions,” he said.
“Looking for these biomarkers, whether or not disease-specific, may also help us find novel pathways that lead to therapeutic interventions.”
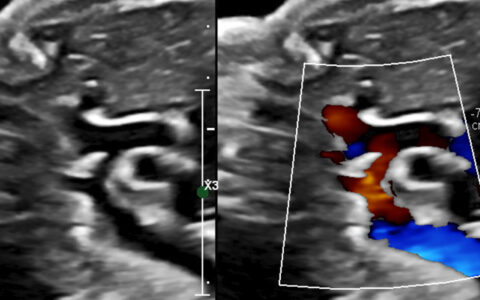
Three other centers will collaborate on the project: Riley Children’s Health, Children’s National Hospital and Nationwide Children’s Hospital. Researchers will do serial evaluations of 200 boys with DMD, at yearly intervals for three years, to articulate the range of phenotypes. Using cardiac MRIs collected at each visit, they will analyze ejection fraction and ventricular volumes, as well as myocardial strain, delayed enhancement (scar), and perform T1, T2 and extracellular volume mapping (looking primarily for diffuse scar and edema). In tandem, they will look for blood biomarkers, tracking changes to see whether they portend future functional changes.
A second goal of the research is to more broadly explore genes in DMD boys, using DNA and clinical history from a larger cohort to look for polymorphisms that may impact the progression of cardiomyopathy. While all boys with DMD share a primary mutation in the DMD gene that leads to a loss of function of the protein dystrophin, many polymorphisms exist that could impact cardiovascular function.
Powering Future Trials
Describing the natural history of the disease will provide critical data to assist researchers with designing DMD trials. Soslow says that knowing how much ejection fraction usually drops or how much their extracellular volume increases over a one-year period is necessary to plan a trial.
“Our overarching goal is to find the right outcome measures that we can use to define the progression so we can design better and smarter trials.”
It will also help researchers choose trial outcomes. “Our overarching goal is to find the right outcome measures that we can use to define the progression so we can design better and smarter trials. With biomarkers that tell us what the patient’s progression is likely to be, we can be more selective in our enrollment and have meaningful drug trials that are smaller and shorter,” Soslow said.