An estimated 1.4 million adults are living with adult congenital heart disease in the United States today, yet only 10% are under the care of a specialized ACHD cardiologist.
These experts offer individualized management aimed at optimizing long-term outcomes for patients with ACHD. Vanderbilt University Medical Center, home to one of the United States’ leading congenital heart disease centers, continues to advance ACHD care through close collaboration among congenital cardiovascular surgeons, cardiologists and imaging specialists who work in comprehensive multidisciplinary teams and utilize the latest technological advancements and medical therapies.
Tetralogy of Fallot: A Lifelong Journey
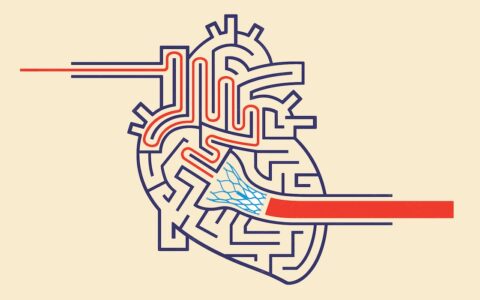
Tetralogy of Fallot, one of the most common congenital heart conditions, disrupts normal cardiac blood flow in babies and results in low oxygen levels after birth. Children with ToF typically require surgical correction during infancy, which has been offered since the advent of open-heart surgery in the 1950s. Though adult survivors of ToF repair require ongoing cardiovascular care, many are achieving normal life expectancy and maintain active lifestyles.
“This used to be called ‘blue baby syndrome,’” said Benjamin P. Frischhertz, MD, co-director of Vanderbilt’s Adult Congenital Heart Disease Program. “Alfred Blalock, MD, and Vivian Thomas, who started their careers at Vanderbilt, along with Helen Taussig pioneered the Blalock-Taussig-Thomas shunt in 1944. The shunt connected the subclavian artery to the pulmonary arteries to improve oxygenation and allowed these children to survive.”
Vanderbilt sees some of the original Blalock-Taussig-Thomas shunt patients who subsequently underwent full repair. They are now in their late 70s and early 80s.
“After tetralogy of Fallot repair, patients require lifelong cardiac care for many reasons,” Frischhertz said. “Surgery often sacrifices the pulmonary valve, resulting in a leaky pulmonary valve and eventually to right ventricle enlargement, which may require a new pulmonary valve. Also, arrhythmia can be an issue in adults with repaired tetralogy of Fallot.”
Valve Management and Emerging Solutions
Historically, some ToF patients could require multiple additional open-heart surgeries for pulmonary valve replacement as tissue valves often degenerate after 10-15 years.
“Not long ago, we did not have any option to replace the pulmonary valve without surgery; however, now we have several catheter-based pulmonary valve replacement options that can be considered for tetralogy patients,” said Robert N. Piana, MD, director of the Adult Congenital Heart Disease Interventional Program.
Newer valve options such as the Harmony and Alterra systems offer non-surgical options for patients with dysfunctional pulmonary valves as well as the dilated right ventricular outflow tracts and pulmonary arteries common after ToF repair. The novel hourglass shape of these valves allows them to anchor securely in place without surgery. Patients recover from their procedures quickly and are usually home they day after implant.
Arrhythmia Management
Tetralogy of Fallot is associated with increased risk of arrhythmia. Post-repair scarring and patches used for the repair can create pathways that allow for ventricular arrhythmia circuits that lead to ventricular tachycardia.
Frischhertz cites a 3-5% lifetime risk of sudden cardiac death among palliated ToF patients, often due to fatal arrhythmias. Currently, he says, about 10% of patients with palliated ToF live with implantable cardioverter-defibrillators.
“Though ICDs are an important safety net, there’s a psychological burden to having this device that could shock at any time to rescue the patient from a dangerous arrhythmia,” he said.
“Bill Stevenson, MD, one of Vanderbilt’s world-renowned electrophysiologists, was the senior author on the first paper to describe these reentrant ventricular tachycardias,” Frischhertz said. Vanderbilt’s ACHD team works closely with the center’s electrophysiology team, including Frank A. Fish, MD, to address these arrhythmias prior to valve replacement, ablating ventricular tachycardia circuits using electrophysiologic catheterization.
“The hope is that we are reducing the risk of ventricular arrhythmia, preventing sudden cardiac death events down the road, and preventing some people from needing an implanted cardiac defibrillator,” Frischhertz said.
Closing the Follow-Up Gap
In ACHD, the follow-up gap is a major challenge. Historically, many patients, especially young adults, fall out of care during transition from pediatric to adult medicine.
Vanderbilt’s ACHD team has led the implementation of a structured transition program with the goal of helping pediatric patients experience a smoother transition to adult medicine and preventing lapses in care.
Training the Next Generation
To address the growing number of adults with congenital heart disease and a national shortage of access to services, Vanderbilt is focusing on expanding its ACHD program. Vanderbilt also offers ACHD fellowship training.
“We’re now training our fifth ACHD fellow,” Frischhertz said. “We’ve deliberately embedded ACHD education and exposure into our division’s teaching program. We hope this engagement leads to interest in residents and fellows who may consider a career in ACHD.”
Vanderbilt’s strength lies in its collaborative approach, he said: “Our seamless collaboration between pediatric and adult interventionalists helps patients across the entire care continuum. We feel this is why Vanderbilt is uniquely positioned to succeed at ACHD.”