Working in Nigeria with local stakeholders, a team of clinician-researchers has created a sustainable program for the primary prevention of strokes in children with sickle cell anemia, a first of its kind for the region. Their work was published recently in Pediatric Neurology.
“Nigeria has more newborns with sickle cell disease than any other country in the world,” said Lori Jordan, M.D., director of the Pediatric Stroke Program at Monroe Carell Jr. Children’s Hospital at Vanderbilt. “About half of the infants with the illness worldwide are born there – about 150,000 newborns each year. Yet the country, and sub-Saharan Africa overall, has never had a sustainable program for the primary prevention of strokes in these children.”
Intensive Stateside Training
“The planning and execution of the stroke prevention program took about eight years,” Jordan said.
Michael DeBaun, M.D., director of the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, led the Vanderbilt team, collaborating with Muktar Aliyu, M.D., Edwin Trevathan, M.D., and others.
“During those eight years, we worked closely with officials in the regional government and provided training at Vanderbilt for a total of 23 Nigerian medical professionals,” Jordan said.
“Sub-Saharan Africa overall, has never had a sustainable program for the primary prevention of strokes in these children.”
Those Nigerian professionals included physicians, nurses, research coordinators, a statistician, and a pharmacist. Key members of the Nigerian team attended the Vanderbilt Institute for Research Development and Ethics program, which offers participants a month of intensive training in research development, as well as training in research ethics and governance. Curricula are tailored for research teams from low-resource settings.
Essential Support from Government Leaders
For the stroke prevention efforts to be sustainable, governmental cooperation was essential.
“They are now beginning to lead their own research studies. This is the best research team I have ever been a part of.”
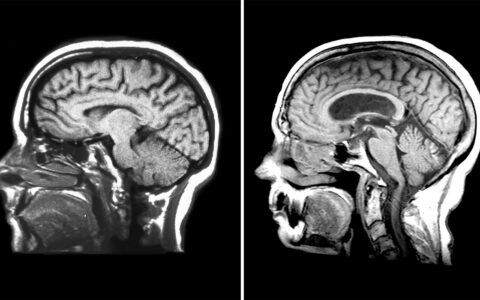
“Public officials in Nigeria agreed to several key steps, including allowing nurses to perform transcranial Doppler (TCD) screenings, where only physicians had been allowed to do so in the past,” Jordan said. “The government also committed to providing free hydroxyurea to children who needed it, based on their having abnormal TCD measurements, once the studies had ended.”
The Vanderbilt group’s efforts were largely funded by the NIH, through its Stroke Prevention in Nigeria (SPIN) trial and its Primary Prevention of Stroke in Children with Sickle Cell Disease in Sub-Saharan Africa II (SPRING) trial. “The SPIN and SPRING trials focus on preventing strokes in children with sickle cell through the use of hydroxyurea for children in northern Nigeria,” Jordan said.
Additional material support included a private donation for the purchase of 10 TCD machines needed for screening.
Obstacles Identified and Addressed
The researchers parsed the obstacles to a successful primary prevention program and devised workarounds for each. One bump was a lack of research experience by local health care providers, which was addressed by a formal training program for the Nigerians at Vanderbilt and includes ongoing mentoring.
“They are now beginning to lead their own research studies,” Jordan said. “This is the best research team I have ever been a part of.”
Another obstacle was the fact that there was only one pediatric neurologist practicing in the area to be served by the prevention program. “To address this issue, one step we took was to provide training to physicians who were not pediatric neurologists in recognizing signs and symptoms of stroke in children,” Jordan said.
Introduction of Electronic Records
For primary stroke prevention to succeed, physicians and pharmacists also needed a reliable platform for communication and maintenance of patients’ active treatment plans. However, electronic prescription systems are rare in low-income countries, Jordan explained.
This led the team to set up an electronic prescriptions system using REDCap to track the use of hydroxyurea and to replace paper prescriptions, which had proven inefficient and inaccurate. REDCap is a free, secure, web-based application designed to support data capture for research studies. It was developed in 2004 at Vanderbilt, with the participation of multiple institutions.
“The Nigerian researchers were able to adopt REDCap with relatively little training, although they also have online tutorials to refer to,” Jordan said. “You don’t need experience with programming or networking to use it.”
REDCap has simple interfaces that capture the necessary prescription details automatically, and it is HIPAA secure, she added.
“One step we took was to provide training to physicians who were not pediatric neurologists in recognizing signs and symptoms of stroke in children.”
Other Technical Adjustments Made as Needed
With high-speed internet service also lacking in the region, the program team devised a way to use the health centers’ Global System for Mobile Communications (GSM) network – a digital mobile network used widely in countries outside the United States. The staff also used personal hotspots on their mobile devices or applied Apple’s AirDrop technology via iPads to allow communication between health care providers and pharmacists.
Jordan is among many Vanderbilt clinicians who have participated in international outreach to low-income communities recently to train child neurologists and other health care workers in the basics of neurological care.