In current clinical practice, there is no effective means of tracking nerve regeneration and growth after repair. Patients and providers must often wait months for evidence of restored motor and/or sensory recovery. When the surgery fails, this translates into a missed opportunity for an early re-operation or other intervention, and a heightened risk of permanent muscle atrophy and loss of function. Diffusion tensor imaging (DTI) may provide a solution.
Diffusion tensor imaging is typically used to examine white matter connections in the central nervous system to diagnose pathologies like traumatic brain injury, spinal cord injury and multiple sclerosis, but it can also elucidate the activity of nerve cells outside of the brain.
In a study published in Annals of Clinical and Translational Neurology, researchers put Diffusion tensor imaging to the test for filling the gap in post-surgical upper limb evaluation. Co-primary investigators Wesley Thayer, M.D., an associate professor of plastic surgery and orthopaedic surgery at Vanderbilt University Medical Center, and Richard Dortch, Ph.D., an adjunct assistant professor of radiology at Vanderbilt, demonstrated that Diffusion tensor imaging was sensitive to differences between damaged and healthy nerves following traumatic nerve injury and compression injuries. In addition, they established that Diffusion tensor imaging could identify failed nerve repairs and successful re-operations.
“It’s used quite a bit in the brain, but our contribution is in translating those methods that have been applied to the brain to peripheral nerves.”
While the study’s focus was on wrists, the ramifications are particularly significant for injuries higher in the arm. “Nerves grow about a millimeter a day,” Thayer said. “In a wrist, there isn’t a lot of time before the nerve innervates the fingers, but in the forearm or upper arm, it takes months to a year to reach them.”
Microstructural Metrics
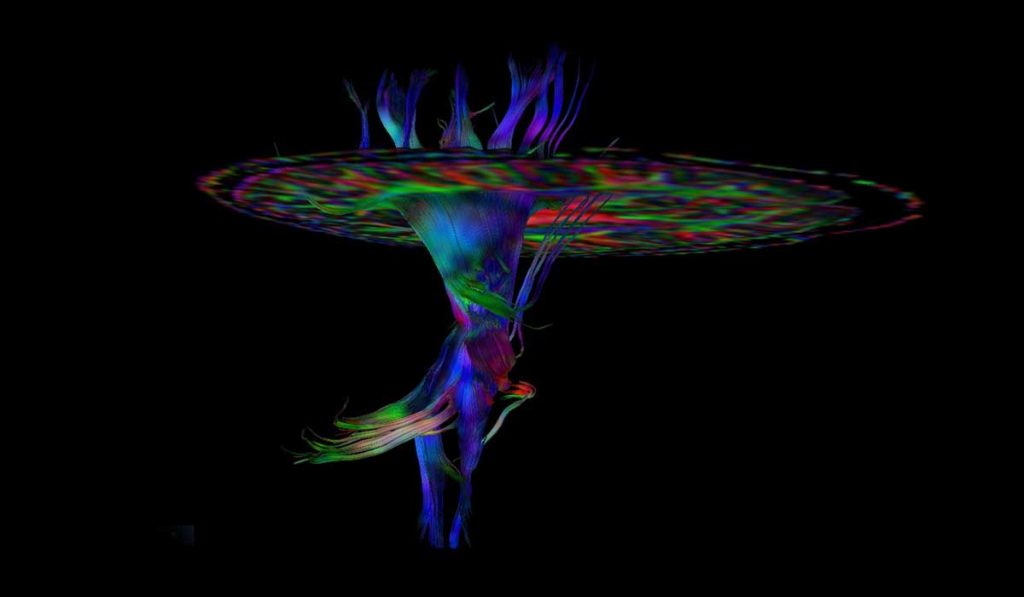
Current imaging methods for peripheral nerves – high resolution ultrasound and magnetic resonance neurography – show only the structure of the nerve and whether the nerve is in continuity. Diffusion tensor imaging can elucidate the status of axonal tracts and their outgrowth following injury and repair.
“DTI is sensitive to the diffusion of water molecules and provides information on tissues at the microstructural level,” Dortch said. “For the elongated cells in peripheral nerves, diffusion is faster along nerve fibers than across them. DTI provides information on this anisotropy, which is altered following trauma and gives us information on how nerves are degenerating or regenerating.”
Dortch adds that DTI capability is a standard MRI vendor offering. “It’s used quite a bit in the brain, but our contribution is in translating those methods that have been applied to the brain to peripheral nerves,” he said.
Sensitivity of DTI Affirmed
In their study, the team tested the capability of DTI to detect failed repairs earlier than current clinical methods. They assessed the degree of nerve repair and regeneration of distal wrist nerves in patients with traumatic nerve injury and followed a separate cohort of patients with compression injury (carpal tunnel syndrome) and healthy controls.
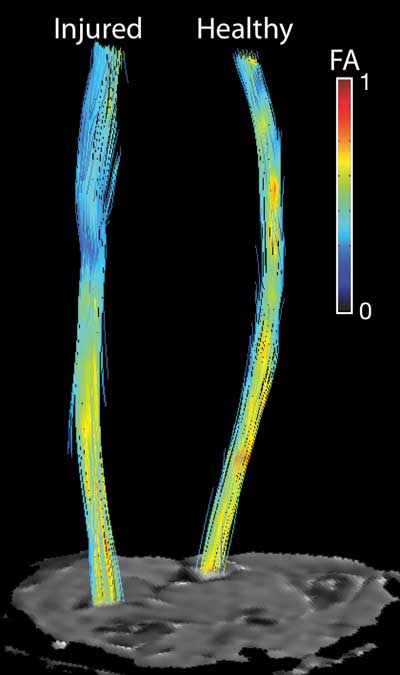
Clinical and MRI measurements were compared to evaluate the relationships between DTI metrics and injury severity. They found fractional anisotropy – a metric derived from DTI – was sensitive to differences between damaged and healthy nerves, damaged and compressed nerves, and injured and healthy contralateral nerves.
“We can detect not only changes related to failed repairs, which represent about 30 percent of nerve repair surgeries, but also the success of reoperations.”
DTI sensitivity was even affirmed in a failed repair, and recovery was noted after reoperation. “First, we watched a drop in our DTI metrics after the first surgical attempt, then after reoperation found that the DTI renormalized to a more anisotropic value consistent with healthy nerves,” Thayer said. “That told us that we can detect not only changes related to failed repairs, which represent about 30 percent of nerve repair surgeries, but also the success of reoperations.”
Pushing the Technology Out
Thayer says this work has potential beyond traumatic injuries. “With some cancers, for example, our ability to repair nerves, coupled with this technology to track recovery, may enable a pivot on many amputation decisions.”
The team is now on the cusp of having protocols in place so that DTI can be used clinically beyond the brain. “We’ve shown that it is feasible and sensitive to degeneration and regeneration,” Dortch said. “I’m hoping that over the next five years, we’ll develop protocols that can be used at any site across any MRI vendor.”
Thayer adds, “We’ve demonstrated that it can guide clinical decisions. Now, we’re working on a multicenter trial as the next step before people start applying this at every hospital.”