Despite significant unrest and deployment of U.S. troops in various regions of the world, the number of trauma cases treated at military treatment facilities (MTFs) has declined both in deployed environments and stateside – the opposite trend of that seen at civilian trauma centers (CIV CENs) in the U.S., where trauma cases have remained steady or increased.
With fewer high-level trauma cases, the U.S. military medical system faces a challenge when training surgeons and maintaining surgical skills, as well as conducting clinical trials, says Lieutenant Colonel Daniel Stinner, M.D., an assistant professor of orthopaedic surgery at Vanderbilt University Medical Center and an active-duty Army officer.
“We need more training on trauma cases, through both clinical exposure or well-developed simulation to ensure that a surgeon has the appropriate knowledge and skillsets to take into the deployed environment,” said Stinner. “The trauma volume at many of our MTF’s just isn’t enough to sustain training.”
“We need more training on trauma cases, through both clinical exposure or well developed simulation to ensure that a surgeon has the appropriate knowledge and skillsets to take into the deployed environment.”
Stinner is leading a partnership between Vanderbilt and Fort Campbell, a U.S. Army installation located 50 miles from Nashville, that is addressing the shortfall in available cases through one of the army’s first military-civilian collaborations to implement a surgical cross-training initiative. Vanderbilt is the only Level 1 trauma center in the Mid-South region.
Evidence-based Trauma Training
A growing body of research demonstrates the importance of military and civilian partnerships for maintaining complex trauma skills. Two such studies were published in Military Medicine in 2017, one of which included work done with the Major Extremity Trauma Research Consortium (METRC), an initiative funded by the U.S. Department of Defense.
The studies compared the number and types of extremity injuries treated at CIV CENs and MTFs and evaluated the viability of cross-training programs at CIV CENs to address current priorities for combat casualty care. Stinner was a co-author on both papers. “Although these studies focused on specific orthopaedic trauma cases deemed essential to combat casualty care, similar results have been shown for general surgery,” he said.
Stinner spends four days each week at Vanderbilt and one day at Fort Campbell’s Blanchfield Army Community Hospital to assist in orthopaedic trauma care and education.
“Because of our long history of partnership with Ft. Campbell and the U.S. Army, as well as a strong commitment from Vanderbilt leadership, our ability to partner with Fort Campbell and become one of the first models of military-civilian collaborations emphasizing trauma care is a natural next step in our relationship,” said Alex Jahangir, M.D., director of the Division of Orthopaedic Trauma at Vanderbilt University Medical Center.
Innovations in Trauma Recovery
Another benefit of the partnership is that it will provide more cases for research. Stinner is the principal investigator on two multi-site trials testing new protocols for orthopaedic recovery.
“A trauma patient’s challenges don’t end with the acute phase of treatment,” Stinner said. “Most patients require rehabilitation and post-acute services to optimize recovery and reintegration back into military service and everyday life.”
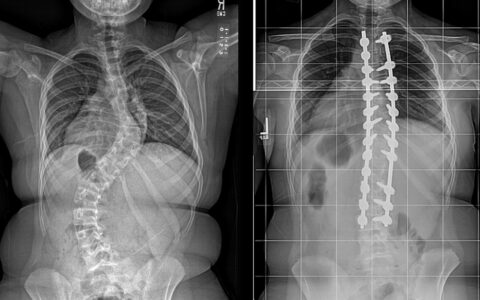
The Rehabilitation Enhanced by Partial Arterial Inflow Restriction (REPAIR) Study, which has now enrolled more than 200 participants, is a prospective, randomized control trial testing blood flow restricted therapy in individuals recovering from a traumatic diaphyseal fracture of the femur. Early Advanced Weight Bearing for Peri-articular Knee and Pilon Injuries (AlterG) will explore the use of an anti-gravity treadmill in patients with distal femur, proximal tibia and distal tibia fractures.
“These are both novel interventions for increasing a patient’s weight-bearing ability,” Stinner said. “The goal is to help them heal faster and return to work (or military duty) faster with better functional muscle mass.”
Bringing ATLS to Ft. Campbell
With the assistance of the Vanderbilt Trauma Outreach Program, Stinner is working towards making Ft. Campbell an official ATLS certification site. The team has helped 15 Army medical providers receive their Advanced Trauma Life Support certification and is planning their next course at Ft. Campbell later this spring.
“We’ve been fortunate to work out this appointment at Vanderbilt,” Stinner said. “These types of partnerships are changing the way we do military medical training, ensuring we remain at the forefront of combat casualty care.”