New research shows the nutritive needs of B cells are more flexible than previously thought, which could enable researchers to steer antibody production in the lymph nodes and spleen to better combat autoimmunity.
Patients with high-risk diseases of the immune system, particularly systemic lupus erythematosus, could stand to benefit from the research findings. Published in the Journal of Immunology, the study provides details regarding how murine B cells use different sugars as they mature into antibody-producing cells.
“Hopefully, we can go beyond B cell depletion or the current standards of therapy in these patients.”
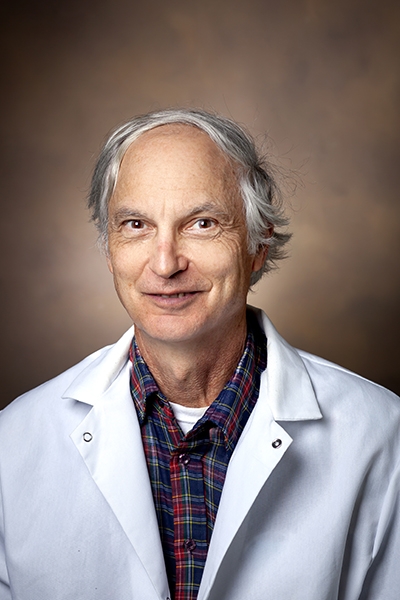
“It has major implications for autoimmune diseases,” said study lead Mark Boothby, M.D., Ph.D., a clinician turned immunologist who led the research out of Vanderbilt University Medical Center. “There’s opportunity here to exploit this metabolic flexibility so, hopefully, we can go beyond B cell depletion or the current standards of therapy in these patients.”
Target Pathway
Normally, B cells transition into plasma cells, which then begin producing antibodies. Regulation of this process goes awry in patients with certain autoimmune diseases, including multiple sclerosis, rheumatoid arthritis, diabetes mellitus, certain cancers, and systemic lupus erythematosus.
Drugs targeting B cells emerged in the 1990s. Rituximab, for one, depletes B cells, preventing them from developing into antibody-producing cells. The goal is to slow down the production process and restore levels of healthy antibodies. The powerful drug is now indicated to treat a host of autoimmune diseases.
“B cell depletion therapy is great. But it hasn’t been great in everything, including lupus,” Boothby said. “We continue to have huge unmet needs for new therapeutics in rheumatology.”
Intake of B Cells
Boothby decided to focus his work where the action lies – germinal centers. These centers, found inside lymph nodes, are an incubator for antibody production. His research team limited the nutrients inside germinal centers to see if they could stem the tide of pathogenic antibody-secreting cells.
Boothby cites the work of his co-author, Jeffrey Rathmell, Ph.D., director of the Vanderbilt Center for Immunology, for showing how it may be feasible to manipulate metabolic pathways within cells in order to change their contributions to disease.
“This is a first stepping stone for us. Could there be ways of manipulating intermediary metabolism, or changing how B cells use nutrients, that would then allow interventions to benefit in lupus?”
Glucose Workaround
In their most recent paper, Boothby, Rathmell and colleagues studied mice genetically engineered to lack glucose transport proteins. Their goal was to see what happens when the mice couldn’t rely on glycolysis to fuel B cell maturation.
“A surprise in our paper is that they can actually get by without glucose to a better extent than one would ever have expected just by giving a couple of alternative sugars,” Boothby said.
The study also showed that, while glucose influx is critical for germinal center homeostasis, manipulated mice can use hexose as alternatives to generate plasma cells and make antibodies. The findings corroborate previous groundbreaking work by Boothby and colleagues that showed germinal centers have a hypoxia response system – a safety mechanism in the case of low glucose.
One-two Punch
“What the paper also shows is if you restrict glucose, you don’t block it completely,” Boothby said. “But, therapeutically, even if we could go from, say, a 12-inch pipe to a 6-inch pipe, it becomes much harder for B cells to become antibody-secreting cells.”
This technique could reduce production of the pathogenic antibody-secreting cells in patients, he said, raising the possibility of combining therapeutic approaches in refractory lupus. This work is ongoing at Vanderbilt.
“We’re trying to do a one-two punch on a pathway that would serve as a bypass route,” Boothby said. “If you were to block the pathway that we’ve studied in the paper, and limit glucose, you could get a very, very dramatic effect.”
The next step is to study both typical and patient-derived B cells to discover how “clamping down metabolic pathways” may modulate the production of antibody-secreting cells, Boothby said.
Long-term, the researchers say this could lead to therapies tailored to an individual’s disease characteristics.
The research is being supported by the National Institutes of Health and Vanderbilt University Medical Center.