Inflammatory cytokines in the aqueous and vitreous of patients with advanced diabetic retinopathy (DR) and diabetic macular edema are encouraging targets in the search for direct biomarkers to predict DR progression and treatment response.
Toward that end, a study launched at Vanderbilt Eye Institute seeks specific inflammatory mediators in the aqueous that are biomarkers for both systemic diabetes and DR progression.
Led by Stephen J. Kim, M.D., Phyllis S. and William B. Snyder Chair and retina division chief, along with co-investigator Sapna Gangaputra, M.D., M.P.H., the INflammatory MediatorS in the PathophysIology of Diabetic REtinopathy (INSPIRE) study is investigating 29 inflammatory mediators that emerged in previous studies worldwide.
“No other study has ever looked at all these markers over time,” Kim said.
Focus On Prevention
Nearly 30 percent of people with diabetes will have some form of DR, with 5 to 10 percent experiencing permanent vision loss. To date, the only validated prognostic DR biomarker is glycated hemoglobin (HbA1C). HbA1C screening, however, reflects glucose control, which indicates disease risk as opposed to DR pathology.
“We screen people with diabetic eye disease and, once they start having vision loss or complications, we can treat them, but from a preventative standpoint we can’t really do anything,” Kim said. “We don’t have a good marker to tell us which individuals will likely develop diabetic retinopathy. Blood glucose and A1C don’t necessarily translate into factors for eye disease.”
The three-year National Eye Institute-funded study follows 164 adults with type 2 diabetes and varying stages of diabetic eye disease – from none to very advanced. A control group of 100 adults without diabetes is also being followed.
Participants visit the Vanderbilt Eye Institute every four months – 10 visits over the life of the study.
“This serial design allows us to show cause and effect, but it requires a real commitment from our participants,” Kim said.
A Multimodal Approach
The study’s central hypothesis is that intraocular inflammatory mediators such as PGE2, IL-6, and IL-8 are markers of DR severity and therefore predict risk of disease progression. Equally important, that they are novel targets for inhibition.
“Our theory is that some of these inflammatory markers are going to correlate with diabetic eye disease, and some of them, hopefully several of them, will predict those who are likely to lose vision,” Kim explained. “If you could show that, you could identify patients who might really have trouble and need early intervention.”
Participants undergo advanced imaging studies (OCT, OCT-Angiography and Optos wide-field) every four months on both eyes to gauge whether DR progression can be predicted from anatomical cues.
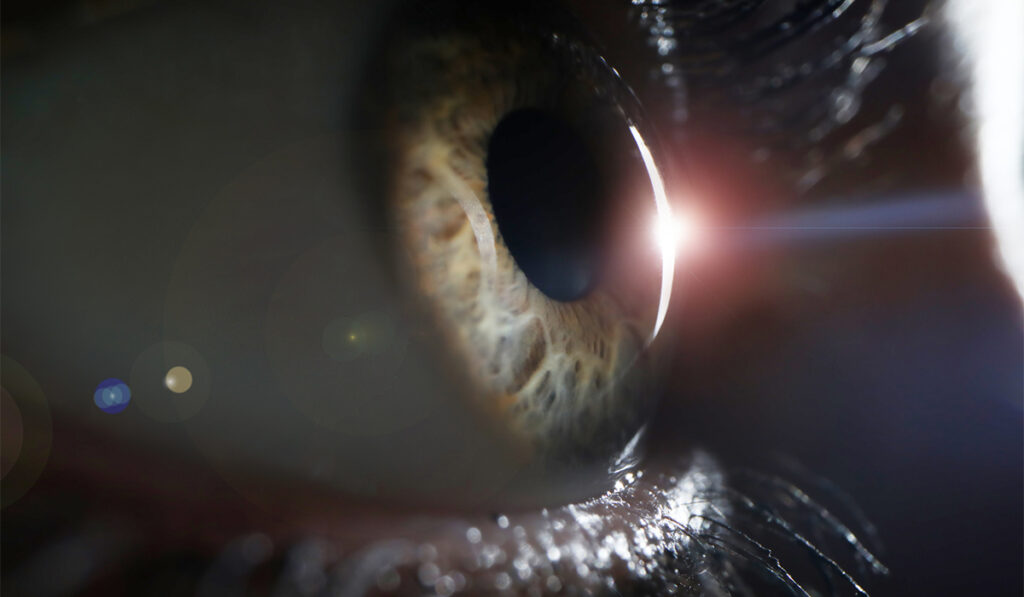
The more invasive part of the study is an aqueous biopsy of each eye, which is required at each visit. Like the vitreous humor, the aqueous reflects localized ocular inflammation. However, the aqueous is technically easier to collect, with less risk.
“We know from this biological fluid that diabetic eye disease is driven by ongoing inflammation and that this inflammation is pathological – it initiates the disease, it propagates the disease, it makes the disease worse. Studying these tissue samples will provide a longitudinal look at this progression,” Kim said.
The study will also determine the long-term effects of sustained ketorolac application on intraocular cytokine levels, DR progression, and diabetic macular edema incidence. Ketorolac, a cornea permeable NSAID, has been previously demonstrated by Kim and colleagues to significantly reduce several elevated inflammatory mediators in DR treatment.
Analyzing the First Wave
Once the investigators have identified the inflammatory targets to inhibit or reduce, they can begin to determine the appropriate treatment for each marker.
“We know all 29 of these markers can be inhibited with anti-inflammatory treatment,” Kim said. “So, once you define the specific disease biomarkers, you have targets to inhibit in a preventative fashion. We may be able to delay diabetic retinopathy complications for years.”
“Once you define the specific disease biomarkers, you have targets to inhibit in a preventative fashion. We may be able to delay diabetic retinopathy complications for years.”
The study will conclude in 2025, but the first wave of patients will begin to exit later this year. Their one-year data will be compared against baseline levels and among the different stages of DR.
Kim believes local inflammation control in the eye will transform future treatment options for diabetic patients facing blindness.
“Tracking and inhibiting these inflammatory mediators has the capacity to reduce or prevent disability in millions of patients every year,” he said.