When Vanderbilt University Medical Center began providing neurology consults via telehealth for community hospitals in Tennessee in 2012, the technology was viewed somewhat skeptically by many payors, patients and physicians.
Later, as the pandemic stretched on with travel constraints and safety concerns, the concept of virtual care became slightly less of a tough sell.
C. Wright Pinson, M.D., chairman of theVanderbilt Health Affiliated Network, continued pushing forward with his vision of extending specialty consults to outlying community hospitals using digital technology. Pinson tasked David Charles, M.D., vice chair of neurology, with developing the first arm of the project: teleneurology consultations.
In time, this early start – accelerated by the pandemic – led to a robust network of consult services across various specialties, including ophthalmology, infectious disease, newborn hearing screening, and EEG interpretations.
“Vanderbilt has relationships with community hospitals throughout Tennessee, northern Alabama, and southern Kentucky, few of which have 24/7 specialty care available,” Charles said.
“One of our main goals is to enable community-based hospitals to keep patients close to their family and home.”
“One of our main goals is to enable community-based hospitals to keep patients close to their family and home,” he said. “Using today’s inexpensive technology, we can do that by dedicating our specialists to as many as 12 hospitals at a time doing bedside consults.”
To date, Vanderbilt’s telehealth physicians have completed thousands of consultations. Surveys following nearly 4,000 teleneurology consults showed 97 percent of patients were highly confident in the care they received, while nearly all clinicians were likely to recommend telehealth to their colleagues. An earlier study of teleneurology consults found that only 13 percent of the patients served through teleneurology were ultimately transferred to a higher-level care center.
“At Vanderbilt, where we operate at full capacity almost every day, we don’t have an incentive to divert all patients to our hospital,” Charles said. “This serves to keep us focused on a streamlined mission, which is to fill a gap right there where the patient and community hospital are located.”
Pandemic as Accelerator
Many Americans live in an area defined by the federal government as having a shortage of health professionals. Because this is even more pronounced in the field of neurology, Vanderbilt launched its telehealth program to address the urgent need for timely stroke evaluation and other emergent care.
Charles says that prior to the pandemic, it was difficult to put telemedicine into play. Limited broadband access and the cost of technology were only part of the problem.
“Insurance companies didn’t want to pay for it, doctors didn’t want to do it, and patients didn’t trust it,” he said. Then the pandemic hit.
“In March 2020, over just eight days, Vanderbilt trained 3,000 faculty and staff in telehealth.”
“In March 2020, over just eight days, Vanderbilt trained 3,000 faculty and staff in telehealth,” Charles said. “We ramped up quickly, going from five to 10 direct-to-patient telehealth visits per day to over 2,000 a day – more than we had done in the entire previous year.”
Today, broadband capabilities are available even in most rural areas, and the skepticism about telehealth has largely been alleviated.
Concern over technology costs also have evaporated.
“In 2012, some community hospitals were using expensive computers on wheels for telehealth,” Charles said. “One of our neurologists suggested we use tablets. After ensuring HIPAA compliance, we rolled out $500 tablets that many community hospitals still use today.”
Clinical documentation can be accessed live on Vitalnet software, where images and test results can be easily shared.
Model of Coordinated Care
Under the telehealth program, each specialty operates on separate financial models with individual agreements.
Some specialties need 24/7 access, while others only require it on weekdays during business hours. The telehealth teams serve cases involving patients who are in the ED, as well as those admitted to the hospital’s ICU or regular hospital units.
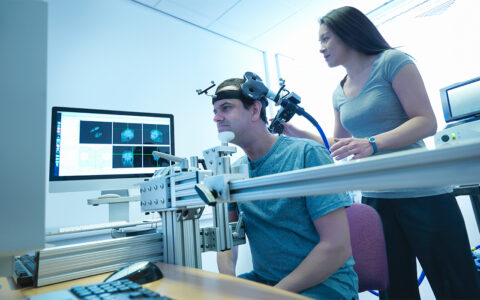
Once the community physician requests a consultation, the Vanderbilt specialist will conduct an exam virtually, with a nurse at the community hospital facilitating. The specialist then formulates recommendations and prepares a clinical document on the case.
Based on the ongoing use of telehealth by community hospitals, Charles predicts other specialties will replicate his department’s use of telehealth.
“I envision a scenario where, as medical director of telehealth, I go to the community hospital with a list of specialties on a one-page document and sit down with their chief executive and chief medical officers,” Charles said. “They could go through that list and select, a la carte, what they need. This may be a few years down the road, but it’s coming.”