A teenage girl from Alabama with a large lateral skull base tumor is among the patients now recovering under the care of two skilled pediatric subspecialists who bring an enhanced level of expertise to the operating room.
Elizabeth Perkins, M.D., director of pediatric neurotology, and Michael C. Dewan, M.D., a pediatric neuro-oncologist and neurovascular surgeon, have been working together to build a strong reputation at Monroe Carell Jr. Children’s Hospital at Vanderbilt for skull base care.
“It’s rare to have two lateral skull base surgeons who focus on pediatrics, a neurosurgeon like myself and a dedicated skull base expert on the ENT side like Elizabeth Perkins, working together on an individual case,” said Dewan, who serves as the surgical director of both the Pediatric Neuro-Oncology Program and the Pediatric Neuro-Vascular Program at Monroe Carell.
Preserving the Patient’s Hearing
In the case of the teenager from Houston, her patient first symptom was a mild hearing loss, which prompted a visit to a community-based otolaryngologist, Perkins explained.
“When her physician got the imaging and saw the tumor, he reached out to me, and our skull base coordinator got her in to see us the very next week.”
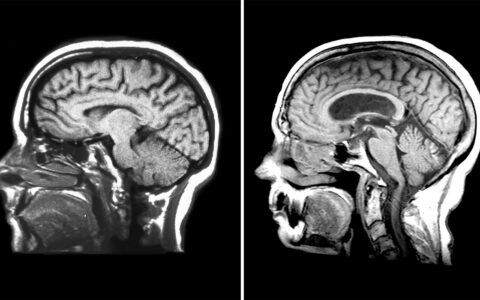
On examination, the subspecialist found that her large tumor surrounded important structures, including the carotid artery and the nerve that controls facial expressions and hearing.
“The tumor was almost eroding into her inner ear,” Perkins said. “She had a high risk of losing all hearing in that ear.”
The tumor was an ossifying fibroma, which a biopsy revealed was not a good candidate for medication that, in certain cases, can shrink skull base masses.
With its high level of specialized expertise, the physicians were able to quickly plan and execute the surgical approach to treatment.
“Our combined abilities allowed us to do an approach that led to a safe, complete resection while protecting vital structures,” Dewan said.
Without a viable drug treatment, a date was scheduled for the surgeons “to go in and go for it all,” Dewan said. The team removed the entire tumor, which was right-sided, with the surgeons performing delicate maneuvers necessary to preserve important nerves, ear bones, and vascular structures.
The 12-hour operation was significantly longer than the more typical 6- to 10-hour skull base procedure and ended with the reconstruction of the patient’s lateral skull.
“Parents are naturally anxious about their children going under for so many hours,” Perkins said. “They want to know that the physicians in charge have the highest level of expertise.”
Dewan added: “She walked out of the hospital two days later, feeling great.”
Skill Sets Combine for Optimal Outcomes
For years, the field of skull base surgery has acknowledged the need for this kind of collaboration for optimal patient outcomes.
In a review article titled “Teamwork in skull base surgery: An avenue for improvement in patient care,” the authors wrote: “It is critical that multiple disciplines work together in order to pool skills, experience and knowledge, and ultimately yield the best patient outcomes.”
Such outcomes are defined as survival and a degree of recovery based on quality-of-life indicators and require time, energy and resources that are not widely available, the authors wrote.
“At our hospital, patients obtain highly coordinated care in an expedited, safe fashion, provided by doctors who are subspecialized specifically to treat children with lateral skull base tumors,” Perkins said.