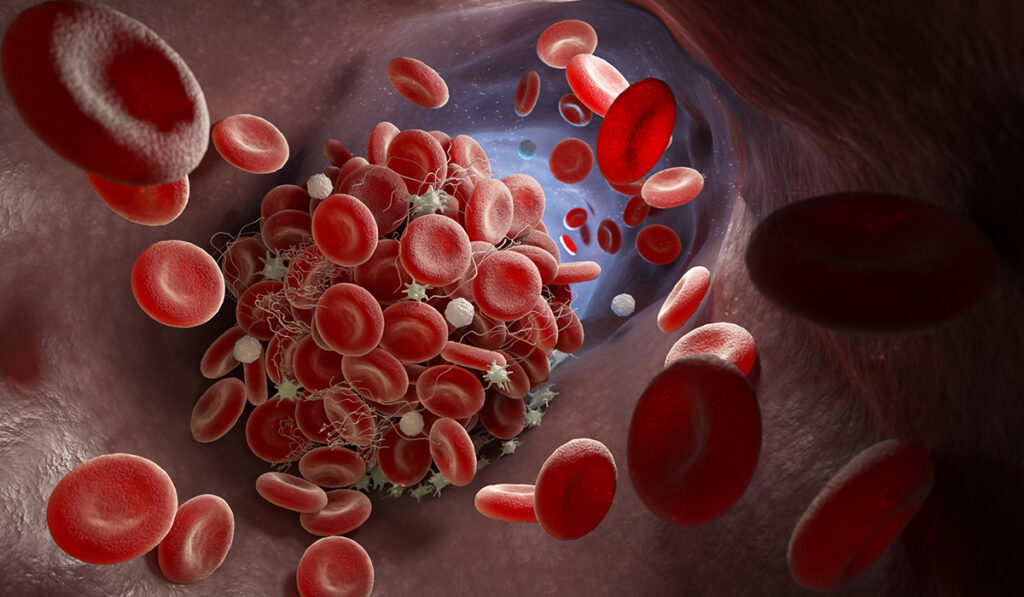
Prothrombotic risks are among the most serious SARS-CoV-2-related concerns. Blood clots afflict many patients with both acute and long COVID. Though rare, clots also have been reported as a side effect of certain vaccines.
While counterintuitive, hemorrhages caused by innate inhibitors to coagulation factors are another real phenomenon related to COVID-19 and the vaccines. General population data from United States sources show that, in rare cases, individuals can develop autoantibodies to coagulation factors. In 20 percent of cases, these responses are associated either with pre-existing malignancy or autoimmune disease.
“I think there’s an enormous amount of crosstalk between coagulation proteins, manipulation of coagulation, derangement of coagulation, and COVID,” said Allison P. Wheeler, M.D., associate professor of pathology, microbiology, and immunology at Vanderbilt University Medical Center. “Complex mechanisms can trigger the coagulation cascade.”
Probing the prevalence of these coagulation inhibitors – predominantly factor VIII inhibitors – Wheeler and colleagues reviewed the medical literature and the CDC’s Vaccine Adverse Event Reporting System (VAERS) looking for answers.
Their findings, published in Research and Practice in Thrombosis and Haemostasis, revealed that reports of coagulation factor inhibitors were rare among those with COVID-19 disease and those receiving COVID-19 vaccines. However, considering how many people have had COVID-19 and may receive additional COVID-19 vaccines in the future, Wheeler says understanding who is at risk remains prudent.
“The vaccine safety message we convey to our patients is punctuated by the fact that coagulation disorders, especially blood clots, after COVID-19 infection are many times more common than in the vaccine.”
The Rare Downside of Heparin
“When someone is acutely ill and hospitalized, heparin is often given to prevent or treat blood clots, but a rare antibody development can paradoxically increase the clotting risk,” Wheeler said.
In this clinical phenomenon, antibodies develop against both heparin and a protein called platelet factor 4. In patients with these antibodies, platelets inappropriately become “stickier,” leading to small clot formation and a decrease in the platelet count. This is opposite of the desired anticoagulatory effect of heparin.
“I think there’s an enormous amount of crosstalk between coagulation proteins, manipulation of coagulation, derangement of coagulation, and COVID.”
This paradoxical event of increased clotting while on an anticoagulant is known as heparin-induced thrombocytopenia (HIT). Very rarely this mechanism can take place in the absence of heparin, in a phenomenon known as spontaneous HIT, where the patient develops antibodies that cause the same effect.
Risks in COVID-19 Patients are Low
To provide insight into the relationship between COVID-19 and hemorrhage, the research team reviewed all documented cases of patients in the United States with autoantibodies specifically directed against blood coagulation factors in the settings of both SARS-CoV-2 infection and vaccination.
“When someone is acutely ill and hospitalized, heparin is often given to prevent or treat blood clots, but a rare antibody development can paradoxically increase the clotting risk.”
Nine of the 15 articles reviewed described coagulation factor inhibitors associated with SARS-CoV-2 infection. As expected, the presence of acquired factor inhibitors led to bleeding symptoms, except in acquired factor XII inhibitors. Forty-four percent of these patients had underlying risk factors for autoantibody formation. One patient who had recurrent hemorrhage expired from cardiopulmonary failure.
Therapeutic interventions to ameliorate bleeding symptoms included recombinant activated factor VII and anti-inhibitor coagulant complex. Immunosuppressive therapy regimens to eradicate the inhibitors were variable, and included rituximab, corticosteroids and cyclophosphamide.
Despite low overall risks, patients with coagulation factor inhibitors are at risk for bleeding, which could worsen if given anticoagulants, as is typically considered in hospitalized patients with acute COVID-19. Wheeler says clinicians need to be aware of the potential for both bleeding and clotting in these patients and to consider derangements in all aspects of the coagulation cascade.
Vaccine Risks Negligible
To investigate vaccine-related risks, the researchers examined VAERS records for potential bleeding episodes or coagulation laboratory abnormalities associated with receipt of a COVID-19 vaccine. This review identified 58 reports of acquired factor VIII inhibitors potentially associated with a COVID-19 vaccine.
Acquired coagulation factor inhibitors were detected in 14 recipients of the Moderna vaccine and 44 recipients of the Pfizer vaccine. Three patients died from hemorrhagic sequelae.
“The risks in the mRNA vaccine are so small that it is safe to say they do not portend a significant increase in either bleeding or clotting risks,” Wheeler said. “The vaccine safety message we convey to our patients is punctuated by the fact that coagulation disorders, especially blood clots, after COVID-19 infection are many times more common than in the vaccine.”