The direct anterior approach (DAA) to total hip arthroplasty has risen in popularity over the past two decades, from only 4 percent of procedures in 2001 to 56 percent in 2019. A research study led by Ryan Martin, M.D., who recently joined Vanderbilt University Medical Center as an associate professor of orthopaedics, offers a head-to-head comparison of post-operative outcomes that may help explain the explosive trend of direct anterior approach.
“Total hip replacement has demonstrated excellent results regardless of which method is used, and many skilled surgeons have consistent success with the posterior approach. In the aggregate, though, our study found superior implant component position with the DAA,” Martin said. “We believe intraoperative imaging helps us achieve optimal positioning more readily, and the fact that we don’t disrupt the posterior hip capsule and musculature helps increase stability resulting in decreased dislocation rates.”
Martin joins a team of orthopaedic surgeons at Vanderbilt who are trained in both anterior and posterior approaches, each performing the surgery of their choice. They plan to extend this line of research by prospectively comparing 2D and 3D imaging studies in DAA and posterior approach (PA) cases to further analyze component positions and other outcomes.
Tackling the Debate
Regardless of the approach, lower dislocation rates and improved wear rates are linked to implants that are more anatomically positioned. Traditionally, most surgeons attempt to position the acetabular components in the Lewinnek safe zone and utilize the femoral component to adjust leg length and offset.
“The fact that we don’t disrupt the posterior hip capsule and musculature helps increase stability resulting in decreased dislocation rates.”
Martin says that past comparative studies have focused on cup position and not the femoral component (with the exception of leg length), even though femoral offset and total offset can substantially affect the function of the hip abductor muscles.
“To our knowledge, no study has compared combined acetabular and femoral implant position outcomes. We asked, ‘Is one approach better at achieving this ideal anatomic implant position?’, which includes cup position as well as restored leg length and offset to the patient’s normal anatomy.” Martin said.
Targets Met More Often
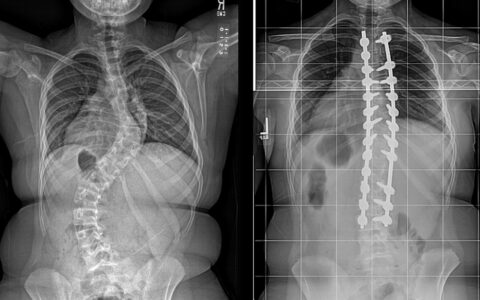
To answer this question, Martin and his colleagues performed a retrospective review of 200 patients who underwent either a DAA or PA procedure. On post-surgical radiographic review, all parameters in the DAA patients were significantly closer to anatomic implant positioning.
“Utilizing anatomic landmarks has inherent variability which can be limited with intraoperative fluoroscopy.”
The DAA cohort achieved more accurate anatomic restoration of leg length (1.6 versus 5.5 mm), femoral offset (4.8 versus 9.3 mm), and total offset (0.5 versus 4.7 mm), compared with the PA. Ideal cup abduction and anteversion were also significantly superior in the DAA (96 versus 78 percent, and 69 versus 24 percent, respectively).
Martin says one of the concerns frequently expressed about DAA is over the accuracy of femoral component positioning. To assess this, the researchers measured both femoral and acetabular anteversion from CT scans and noted that they were able to achieve ideal implant placement reliably with the DAA approach.
Better Visibility
Martin says the convenience of intraoperative fluoroscopy provides inherent guiderails for the procedure, the most dominant factor in the findings of aggregate superiority. In PA procedures, Martin explains that fluoroscopy is cumbersome because the patient is in a lateral (versus supine) position. In its absence, a standard X-ray is often necessary, adding significant time delays and making it more difficult to achieve an ideal image of the patient’s pelvis/hip.
He also cites the potential advantage of the anterior approach in avoiding disruption of the posterior soft tissues. “Disruption of the posterior soft tissues can decrease stability of the hip, potentially resulting in a hip dislocation. Increasing offset and leg length are surgical methods for decreasing this risk but may make it more difficult to achieve anatomic implant position with the posterior approach,” Martin said.
“Utilizing anatomic landmarks has inherent variability which can be limited with intraoperative fluoroscopy,” he added.
“With DAA, the imaging helps us place our instruments, do live templating and confirm the position of our implants. I can put in my cup and view various different femoral components on X-ray or on the fluoroscopic image, including a side-by-side comparison with the contralateral hip. With DAA, I can leave the OR confident I’ve hit my mark.”