The bulk of diabetes research has focused on how to replace insulin action to control blood glucose in both type 1 and type 2 diabetes. A team of researchers across several academic medical centers are shifting the focus to another angle, looking at glucagon as a cause of high blood glucose. In doing so, the researchers made the surprising discovery that blocking glucagon signaling under diabetic conditions promoted the conversion of α-cells into insulin-producing β-cells.
In the Proceedings of the National Academy of Sciences, the research team reported that using monoclonal antibodies to block glucagon receptors in type 1 diabetic mice promoted survival, lowered glycemia, and significantly enhanced circulating insulin and C peptide. Importantly, this regeneration took place in human pancreatic islets implanted in the mice, auguring translational potential.
“Seeing signs that functional mass improved in these xenografts is extremely encouraging,” said Danielle Dean, Ph.D., an assistant professor of medicine at Vanderbilt University Medical Center, and a study author. “Expanding even small amounts of residual β-cells can greatly improve quality of life for millions of patients with type 1 diabetes,” she said.
Glucagon’s Multifaceted Role
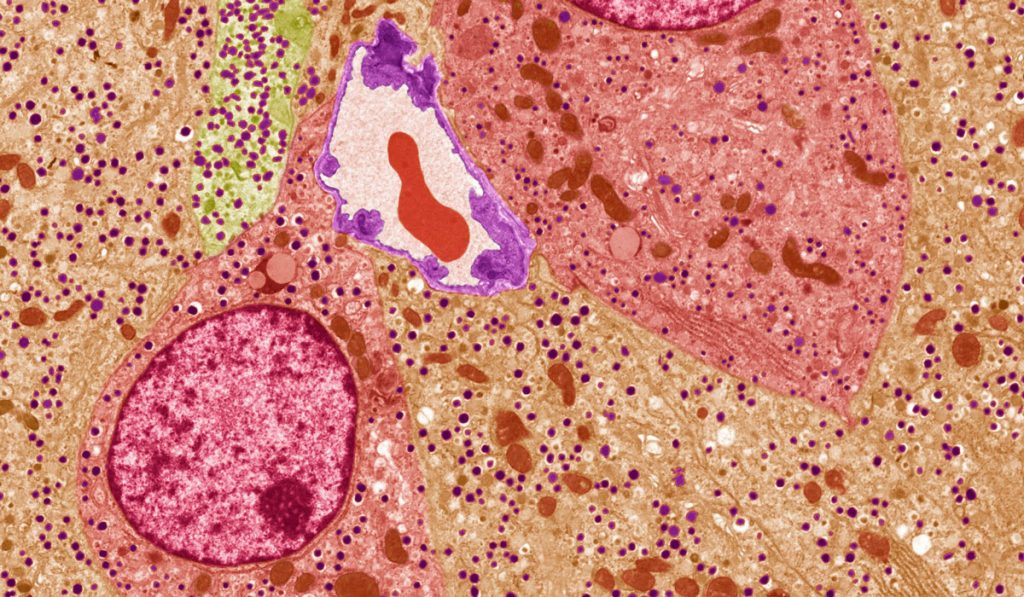
Produced by the α-cells in the pancreatic islet, glucagon stimulates the liver to release glucose and raise blood sugar levels. In people with diabetes, β-cells, also found in pancreatic islets, do not produce enough (if any) insulin to promote the uptake of glucose from blood, and they also fail in their role of suppressing excess glucagon. This combination leads to unstable glycemic control.
Dean says that glucagon’s role in diabetes has not received the research focus of other hormones and mechanisms. “While blocking glucagon to lower blood glucose as a strategy to treat diabetes makes intuitive sense, it can trigger a cascade of unintended consequences,” she said. “By lowering glucagon, the liver produces signals to make more glucagon. It also stimulates α-cells to proliferate, resulting in hyperplasia.”
“One of the things that is remarkable about this study is we do see effects on human islets – we see signs that they may be regenerating.”
While this side effect has delayed or even derailed the clinical development of this treatment strategy, “we found previously that it is evidence of a strong endocrine feedback loop between the liver and α-cell,” Dean explained. The new study suggests using a glucagon-blocking strategy instead could have a stabilizing effect over time and help the body improve its own capacity to secrete insulin.
Promising Results
The study tested the hypothesis that monoclonal antibody antagonists of the glucagon receptor (mAb-4) help maintain glucose homeostasis in mice with type 1 diabetes. The mice were first allowed to become overtly hyperglycemic. Then the test group was treated with mAb-4 and the control group received immunoglobulin for several weeks.
Study authors observed “durable and sustained improvements in glycemia, which persisted long after treatment withdrawal,” in the test group. Antibody treatment promoted the conversion ofα-cells to β-cells in the mouse pancreas, which increased 6.7 fold. Mice that received human islet xenografts also showed lasting improvements in human insulin secretion.
“It appears that our intervention stimulated production of insulin-positive β-cells from α-cell precursors at least in the mouse pancreas,” Dean said. “This increase in β-cell mass from glucagon receptor antagonism has been observed not just in mouse models of type 1 diabetes but it in type 2 as well.”
Exploring Translational Potential
“We have cured diabetes in mice many times over, but translation to humans has been disappointing,” Dean said. One of the things that is remarkable about this study is we do see effects on human islets – we see signs that they may be regenerating.”
Next, the researchers want to determine if a greater quantity of human β-cells can be generated as a result of glucagon receptor antagonism, and human α-cell precursors can take on insulin-secretory functions under these conditions.
“Ultimately if you are going to cure type 1 diabetes, you need to replace the β-cells and mitigate the immune attack on those β-cells. A tall order, but these are the types of studies that might be going in that direction,” Dean said.