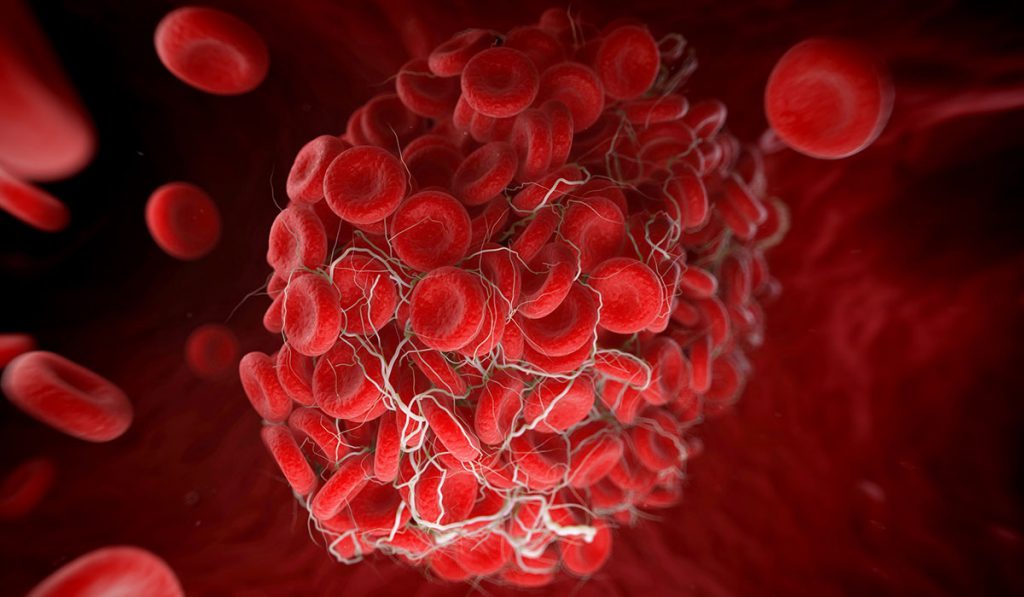
Researchers have identified a key biomarker to predict patients at high-risk for developing venous thromboembolism (VTE) in pediatric musculoskeletal infections (MSKIs), a significant step toward preventing morbidity and mortality from a dangerous complication.
“There are no measures that permit a treating physician to determine which child with musculoskeletal infection is at risk for thrombosis and can therefore be treated prophylactically,” said Jonathan Schoenecker M.D., an associate professor in the Division of Pediatric Orthopaedics at Monroe Carell Jr. Children’s Hospital at Vanderbilt.
Schoenecker is lead investigator on the study, published in the Journal of Pediatric Orthopaedics, reporting that levels of C-reactive protein (CRP) during the body’s acute phase response (APR) to injury are strongly correlated with risk of VTE. The findings suggest that if CRP levels can be tested during APR, physicians can better risk-stratify patients and take preventative measures sooner to prevent VTE from developing.
The research team’s studies suggest levels of CRP may also prognosticate whether a patient has been treated adequately following surgical debridement, or if they require escalated management, such as further debridement or broader antibiotics, to reduce risk of complications.
Pharmacologic Prophylaxis for MSKI Patients
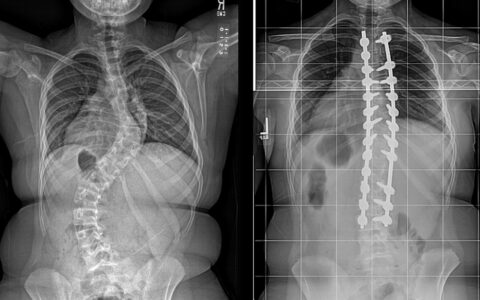
For their study, Vanderbilt researchers did a retrospective review of patients 18 years of age or younger who had an orthopaedic consult for MSKI from 2008 to 2013. Pediatric patients with MSKIs are at significantly higher risk of VTE than the general population.
CRP was used as the measure of APR as it is a well-known pro-inflammatory reactant and pro-coagulant during APR. “The acute phase response is the hormonal system that resolves problems created by injury,” Schoenecker explained. CRP values were assessed from the time of admission until CRP normalization or discharge.
Overall, peak CRP elevation was strongly linked to risk of VTE, and the correlation existed independent of patient age. A 20 mg/L increase in peak CRP correlated with a 29 percent increased risk of VTE, with the risk continually rising as CRP levels increased.
The researchers concluded pharmacologic prophylaxis should be considered for MSKI patients going through APR and that evaluative studies are needed.
Monitoring CRP to Assess Treatment Efficacy
Ongoing research from Schoenecker and colleagues suggests that changes in CRP after surgical debridement of an MSKI is a single determinant that indicates if escalation of medical and/or surgical management is required.
In a recently completed a review of 135 pediatric MSKI patients, the investigators found that patient care teams commonly increased the number of antibiotics administered and provided further surgical intervention when CRP levels increased 48 hours postoperatively or when a patient’s preoperative CRP was over 90 mg/L. This work was presented in part at the 2020 Pediatric Orthopaedic Society of North America annual meeting and the Orthopaedic Research Society annual meeting.
“This is the first study to evaluate the clinical utility of utilizing repeated measures of the acute phase reactants (CRP) after an intervention (surgical debridement) as a measure of the adequacy of reducing the severity of the infection and therefore the risk of adverse outcomes,” Schoenecker said.
A Widely Applicable Biomarker
The Vanderbilt researchers further hypothesized that using CRP to measure APR can be applied across disease states and patient populations. CRP has previously been found to be associated with increased risk of VTE for adult cancer patients.
“As serial CRP measurements become standard of practice, future prospective studies are needed to optimize the timing of CRP reassessment during inpatient hospitalization, weighing both improvement of patient care and clinical burden,” Schoenecker said.