The Vanderbilt Memory and Aging Project (VMAP) has won an $18.2 million grant renewal from the National Institute on Aging to continue studying the role of vascular changes in the onset and progression of Alzheimer’s disease. This work offers hope for early prevention.
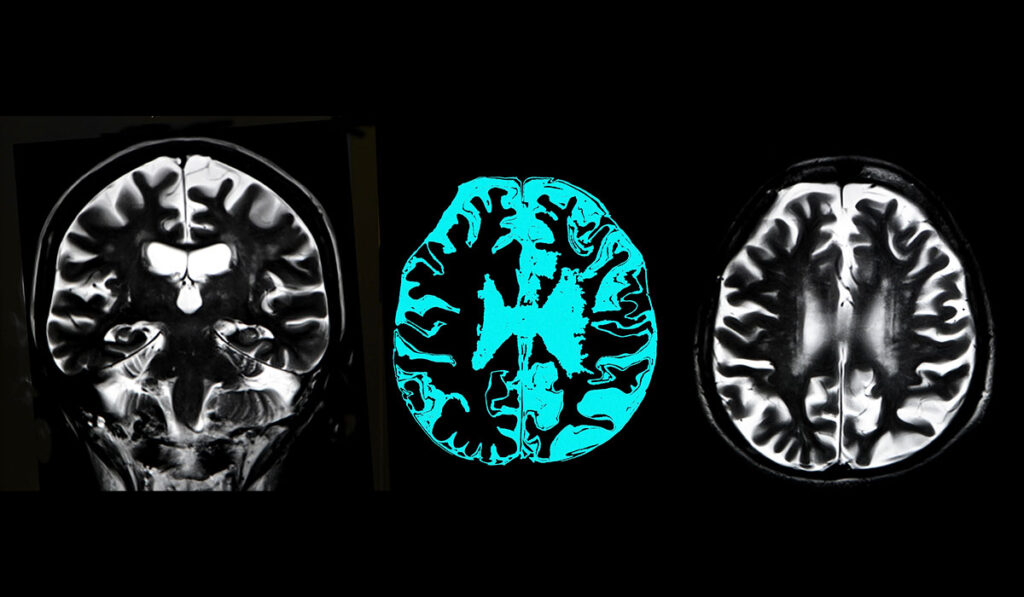
For decades, Alzheimer’s research has focused on the role of amyloid plaques and neurofibrillary tangles in age-related memory loss. Increasingly, though, researchers are realizing that impaired circulation plays a large role in cognitive decline.
“Compromises in cerebrovascular health may be an unrecognized driver of phosphorylated tau, which is much more tightly linked to cognitive decline than amyloid plaques,” said Angela Jefferson, Ph.D., director of the Vanderbilt Memory and Alzheimer’s Center and principal investigator for VMAP. Furthermore, Jefferson notes, the cerebrovascular compromises involved in memory loss are largely driven by modifiable risk factors.
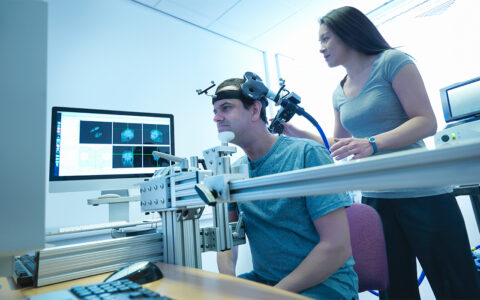
VMAP, a longitudinal investigation of vascular health and brain aging, began in 2012 with a cohort of 335 community-dwelling participants ages 60 to 92. The grant renewal will allow the researchers to expand the cohort to include more than 900 participants, making VMAP the largest study of its kind.
New Prevention Possibilities
While rates for other major causes of death are declining, the national mortality rate for Alzheimer’s has been climbing for years. It rose 146 percent between 2000 and 2018, illustrating the urgent need for scientific breakthroughs in prevention and treatment.
Jefferson’s research team is leading the way in cultivating understanding of how age-related cardiovascular and cerebrovascular changes drive memory loss. “With growing recognition that the pathological hallmarks of Alzheimer’s disease develop 20 to 25 years prior to symptoms emerging, the potential for preventive efforts centered on vascular health take on heightened importance,” she said.
A detailed understanding of how age-related cardiovascular and cerebrovascular changes drive memory loss offers enormous potential for large-scale prevention opportunities. Said Jefferson, “Proven approaches that reduce vascular risk factors, preserve cardiovascular health, and prevent heart disease may also support cerebrovascular health and prevent Alzheimer’s disease. There are huge public health implications to this heart-brain connection that links vascular health and cognitive decline.”
“Proven approaches that reduce vascular risk factors, preserve cardiovascular health, and prevent heart disease may also support cerebrovascular health and prevent Alzheimer’s disease.”
Intervening Early and Reducing Disparities
Cerebrovascular changes are a common pathology to co-occur with Alzheimer’s disease, and findings from the initial VMAP funding period suggest cerebrovascular changes may even precede Alzheimer’s disease onset.
The expanded VMAP study has three goals: (1) determine if changes in vascular health and hemodynamics precede abnormal protein changes linked to Alzheimer’s disease and dementia pathology; (2) determine if such changes precede the onset of cognitive and memory loss symptoms; and (3) determine if genetic susceptibility to Alzheimer’s disease exacerbates connections between vascular health issues, Alzheimer’s protein changes and symptom onset. To achieve these goals, the study will characterize co-occurring pathological processes in middle-aged adults, a group Jefferson says is often understudied in Alzheimer’s disease.
In addition, understanding and reducing disparities in Alzheimer’s disease and cognitive decline will be an important focus. Black/African Americans have an increased risk of developing Alzheimer’s disease than their white counterparts. Vanderbilt Memory and Alzheimer’s Center faculty have pioneered new ways to engage older African Americans in research opportunities and will work to build a more diverse and representative VMAP cohort.
The Center is also studying sex-specific differences in Alzheimer’s disease. Women represent two-thirds of Alzheimer’s cases, and Vanderbilt Memory and Alzheimer’s Center scientists have shown that Alzheimer’s manifests differently in women and men. Said Jefferson, “Thus, the VMAP expansion will provide important opportunities to learn much-needed information about potential prevention and therapeutic pathways for precision medicine.”