An increasing number of children and adolescents, predominantly girls, experience frequent nausea that is not attributable to an underlying disease. Functional nausea (FN) can lead to multiple long-term difficulties into young adulthood due to anxiety, depression and GI distress.
At Monroe Carell Jr. Children’s Hospital at Vanderbilt, specialists across adolescent medicine, adult surgery, psychology and pediatric GI are working to make FN diagnosis simpler and more accurate.
“To date, there has been no tool to quantify and measure functional nausea,” said pediatric gastroenterologist and researcher Alexandra Russell, M.D., director of the pediatric nausea clinic at Vanderbilt. “We have visual scales for rating how bad the nausea is, but nothing that tells us what is happening on the inside.”
“We have visual scales for rating how bad the nausea is, but nothing that tells us what is happening on the inside.”
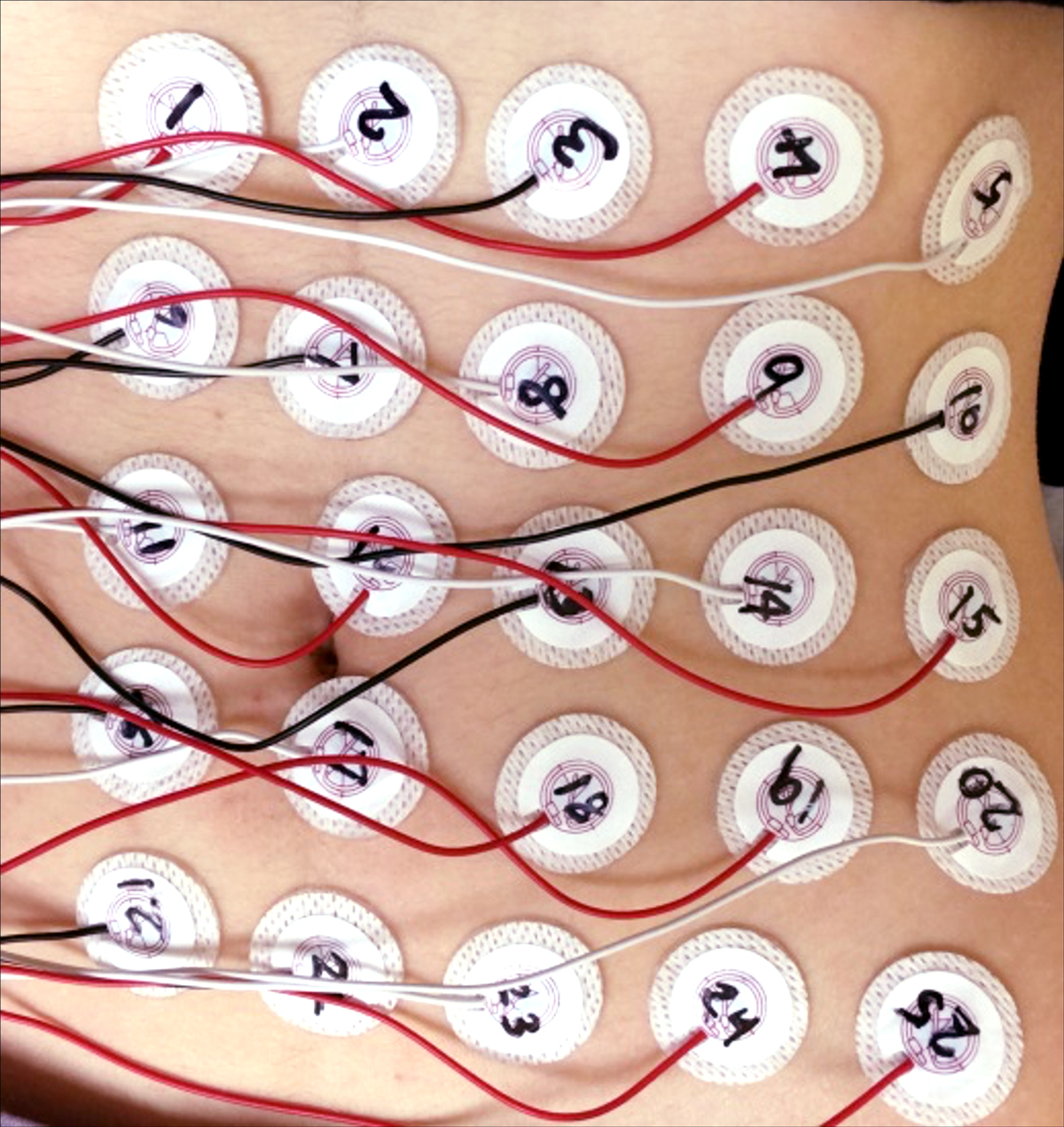
Russell’s team has repurposed non-invasive GI tools and are testing their sensitivity to the gastric electrical activity associated with FN. In a preliminary study using electrogastrograms (EGGs), FN patients, post-prandial, demonstrated disordered propagation compared to healthy controls, a predominantly retrograde pattern, and indications of gastric uncoupling. These results suggested their new approach may enable the distinctions needed to refine FN diagnosis, evaluate treatment and target new therapies.
An Insidious Cycle
Functional nausea typically afflicts children and adolescents ages eight to 17 years, and can be debilitating. While vomiting does not routinely accompany FN, Russell notes sufferers have a prevailing sense of imminent vomiting, localized either in their stomach or the back of their throat, exacerbated by the smell and sight of food.
Whether a predilection toward anxiety triggers FN or vice versa is difficult to discern. “The nausea cycle may be kicked off by an illness, a medication or a stressor,” Russell said. “Then they tend to ruminate on that nausea, worry that they will vomit, and that anxiety fuels the cycle.”
The most successful treatment for FN to date has been low dose antidepressants. Tricyclics or SSRIs, which help regulate motility and sensitivity in the gut and reduce anxiety, can help break the rumination cycle in some patients.
New Measurement Tools
Standard EGG and magnetogastrogram (MGG) have limited powers of discrimination between normal and abnormal gastric propagation. Russell and her fellow researchers have customized their high-resolution electrogastrogram (HR-EGG) with 25 electrode channels for characterizing gastric slow waves by frequency, distribution of spectral power, spatiotemporal frequency maps and slow-wave propagation patterns.
Using HR-EGG and MGG together reveals isolated patterns of activity in the gut. Russell’s preliminary study included ten FN patients and ten controls who underwent multichannel HR-EGG/MGG to evaluate spatiotemporal slow-wave parameters, pre- and post-prandial.
Post-prandial, FN patients demonstrated faster propagation than healthy controls, a predominantly retrograde pattern, and indications of gastric uncoupling.
“Understanding the major pathophysiologic mechanism underlying FN might allow cause-specific therapeutic interventions, which will be our main focus in future studies,” Russell said. “Treatment during a time of therapeutic plasticity may prevent the long-term morbidity we have seen in this patient population.”
“Now we are starting to describe FN as a disease of slow wave rhythm disturbances.”
Exploring the Tools’ Utility
The team is now working with a larger cohort to fully assess the tools’ clinical utility. They will evaluate how the multichannel HR-EGG/MGG discriminates between patients with FN and controls, pre- and post-prandial, and look at differences when the condition is medicated.
Russell also plans to investigate pattern distinctions between FN patients who are symptomatic and asymptomatic, and whether these correlate with symptom severity, functional disability, quality-of-life measures and psychological functioning. Further, they will explore how EGG and MGG rhythm and propagation abnormalities in FN patients correlate with psychological functioning.
“Patients have often been told it is all in their head,” Russell said. “Now we are starting to describe FN as a disease of slow wave rhythm disturbances. Now, they can say, ‘Yes, I really do feel terrible, but it’s because there really is something wrong with me.’”