Primary outcomes of the ISCHEMIA study, announced at the 2019 American Heart Association Scientific Sessions, placed medical management on par with percutaneous coronary intervention or surgery for patients with stable cardiovascular disease. The results either surprised or confirmed the beliefs of many providers. However, the question remains as to whether it constitutes a clinical game-changer.
Daniel Muñoz, M.D., associate executive medical director at the Vanderbilt Heart and Vascular Institute, calls the study “very important,” but says it needs to be clearly contextualized for clinical practice. “We need to guard against people categorically debunking stenting or surgery,” he said.
“We need to guard against people categorically debunking stenting or surgery.”
The Study
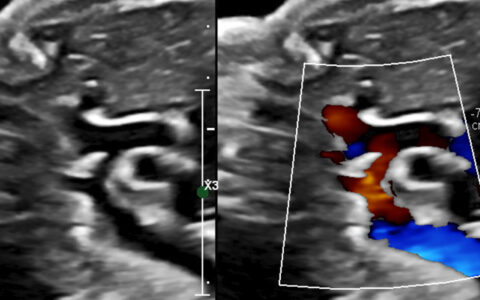
ISCHEMIA researchers enrolled 5,179 adults with stable cardiovascular disease at 320 sites around the world. All participants had at least three ischemic segments with less than 50 percent occlusion, as confirmed through imaging tests. Severity of angina varied from none (34 percent) to daily/weekly episodes (22 percent).
One randomized cohort received percutaneous catheter intervention (balloon and stent) or coronary artery bypass grafting plus medical management, and a second received only medical management. Medical management was individually prescribed to each participant, regardless of what drugs, if any, they were taking upon enrollment.
After following these patients for an average of 3.3 years, researchers found that the risk of recurrent heart attack, stroke or all-cause mortality did not differ significantly between the two groups.
Changing the Conversation
Muñoz says that the outcome is more aptly termed a “conversation-changer” than “game-changer.” What once prompted a fairly routine referral for a stent, for example, will now call for thoughtful shared decision-making. Patients with stable angina will need to decide whether risks of a procedure are worth the benefits of chest pain relief, which was significant in the study.
Patients with stable chest pain symptoms who got stents reported a 70 percent decrease in pain, versus 40 percent for the medical management only group. “It is very fair to say to patients that revascularization through stenting or bypass is likely to result in improvement or resolution of your symptoms. What we can’t say is that you are going to live longer or that this is going to lower your chances of having a heart attack down the road,” Munoz said.
Muñoz expects the ISCHEMIA outcomes to make treatment of stable patients more consistent and more conservative. “I think clinicians will more consistently pause before proceeding with invasive procedures for patients with stable ischemia. That pause should importantly involve a conversation between a patient and their doctor,” he said.
Colin Barker, M.D., Vanderbilt’s director of interventional cardiology, shares Muñoz’s views. “For most cardiologists, the trial will not be practice-changing. The therapies – medicines and stents – are complementary, as underscored by the fact that 23 percent of the medical management patients crossed over to intervention over the study period,” he said. “For those with persisting symptoms or who have trouble with medicines, the choice of intervention for symptom relief and improved quality of life makes sense.”
Questions for Substudies
“There is no substitute for great data and a well-done study, and this ISCHEMIA trial is both.”
Providers can anticipate further guidance following the subanalyses, which are likely to be prolific in a study as large and data-rich as ISCHEMIA. Among the variables ripe for parsing are a type of lesion, number of lesions, arteries affected, history, exercise and diet and other risk factors.
As Barker points out, ISCHEMIA’s primary outcomes do not incorporate the fact that almost one-quarter of the patients assigned to medical therapy alone wound up with a revascularization intervention over the follow-up period. A close look at the patients who had these interventions could impact study interpretation and clinical implications.
The effect on reimbursement is another unanswered question. With 17 million Americans living with stable heart disease, the cost-savings from foregoing interventional procedures are estimated at over half a billion a year. Clinicians may need to adjust to new coding regimens as the justifications for performing a procedure shift.
The primary outcomes are strong enough, however, to prompt offering these patients alternatives that were previously considered contraindicated. “There is no substitute for great data and a well-done study, and this ISCHEMIA trial is both,” Muñoz said.