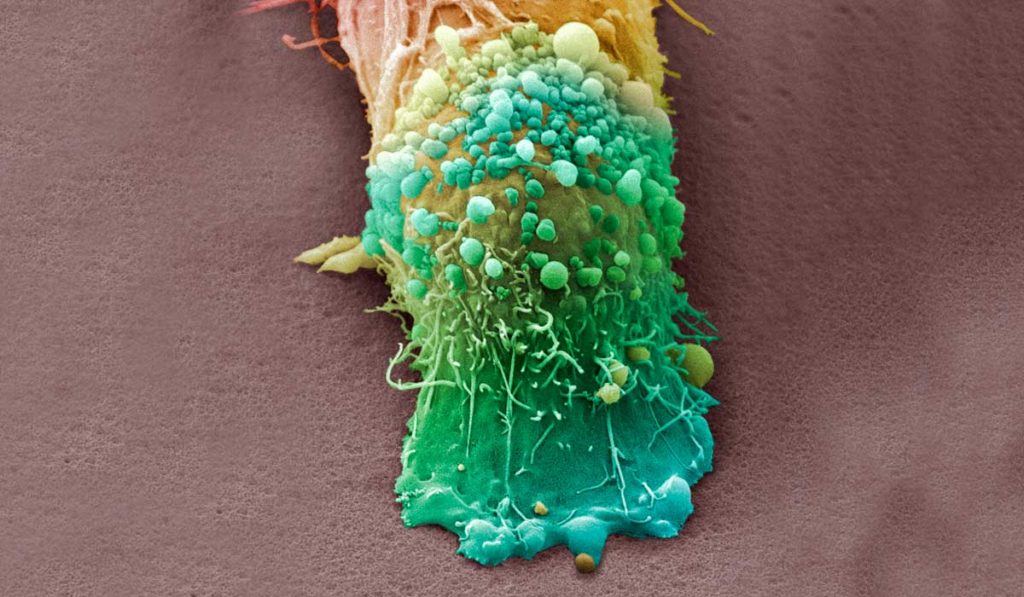
Roughly half of all melanoma patients are unresponsive to immunotherapy as a first-line treatment for metastatic melanoma. Targeted therapies can be effective, but patients often acquire resistance. There remains an urgent need to develop new therapeutic approaches.
A new study from the Vanderbilt-Ingram Cancer Center published in the journal Science Translational Medicine has identified a potential melanoma therapy treatment that would pair inhibitors of cyclin-dependent kinases 4 and 6 (CDK4/6), which are currently used for the treatment of breast cancer, with antagonists of murine double mutant 2 (MDM2).
“We were specifically looking to develop second-line treatment for melanoma patients who are not responsive to current standard-of-care therapies,” said Anna Vilgelm, M.D., lead author on the publication and research assistant professor of pharmacology at Vanderbilt University Medical Center at the time of the study. Ann Richmond, Ph.D., Ingram Professor of Cancer Research at Vanderbilt, co-led the study.
Resistance to CDK4/6 Inhibitors
Two cell cycle kinases, CDK4 and CDK6, are often constitutively activated in melanoma tumors due to genetic alterations of CDKN2A. “More than 40 percent of melanoma tumors exhibit loss or mutation of CDKN2A, a gene that regulates CDK4/6 and MDM2 to control cell cycle,” Richmond said.
“Therefore, we thought that CDK4/6 inhibitors may be effective against melanoma, because melanoma tumors will be dependent on CDK4/6 for their growth,” Vilgelm added. “When we tested this in our model, it turned out that most of the melanoma tumors were actually resistant to the CDK4/6 inhibitor as a single agent.” They then went on to investigate the mechanism of resistance.
Overcoming the Resistance
Using genetic and proteomic analysis of 13 melanoma patient-derived xenografts, the team determined that CDK4/6 inhibitor-resistant tumors commonly displayed activation of the phosphatidylinositol 3-kinase (PI3K)-AKT pathway.
“We were able to analyze what genetic and protein markers are associated with resistant and sensitive tumors.”
“We were able to analyze what genetic and protein markers are associated with resistant and sensitive tumors,” Vilgelm explained. “From the proteomic analysis, we knew to look more closely at the PI3K-AKT axis, and at p21.”
The research team determined that the PI3K-AKT pathway in CDK4/6 inhibitor-treated cells causes inhibition of p21. A key function of p21 is to inhibit the cell cycle protein, CDK2. With p21 inhibited, CDK2 is left unchecked to promote cell cycle progression, permitting CDK4/6 inhibitor-treated cells to develop resistance by relying on CDK2 for proliferation.
Having shown that inactivation of the CDK inhibitor p21 promotes CDK4/6 inhibitor resistance, Richmond and Vilgelm sought to pharmacologically induce p21 expression in order to overcome the resistance. MDM2 antagonists can induce p21 by stabilizing p53, a driver of p21 transcription. The study reports that coadministration of CDK4/6 inhibitors with MDM2 antagonists inhibits melanoma growth both in vivo and in an ex vivo model.
An Effective Therapeutic Combination
Vilgelm and Richmond are excited that this therapeutic combination could be a second-line choice for patients who do not respond to current standard-of-care melanoma therapies and hope to see this study move further into clinical development.
“Our finding, that combining a CDK4/6 inhibitor with an MDM2 inhibitor can overcome this genetic driver of melanoma, i.e., mutation or loss of CDKN2A, is very promising and should be tested further in clinical trials,” Richmond said.
Vilgelm also emphasized the strength of the research approach to unravel mechanisms of resistance to existing inhibitors. “Using clinically relevant models, looking at genetic and proteomic markers of the tumors, and comparing these markers with response can really give us information on the mechanism and identify potential partners for effective therapeutic combination.”